Read More >
- Anterior Ankle Impingement - July 24, 2022
- Tarsal Coalition - October 12, 2022
- Sural Nerve Pain - October 3, 2022
Anatomy
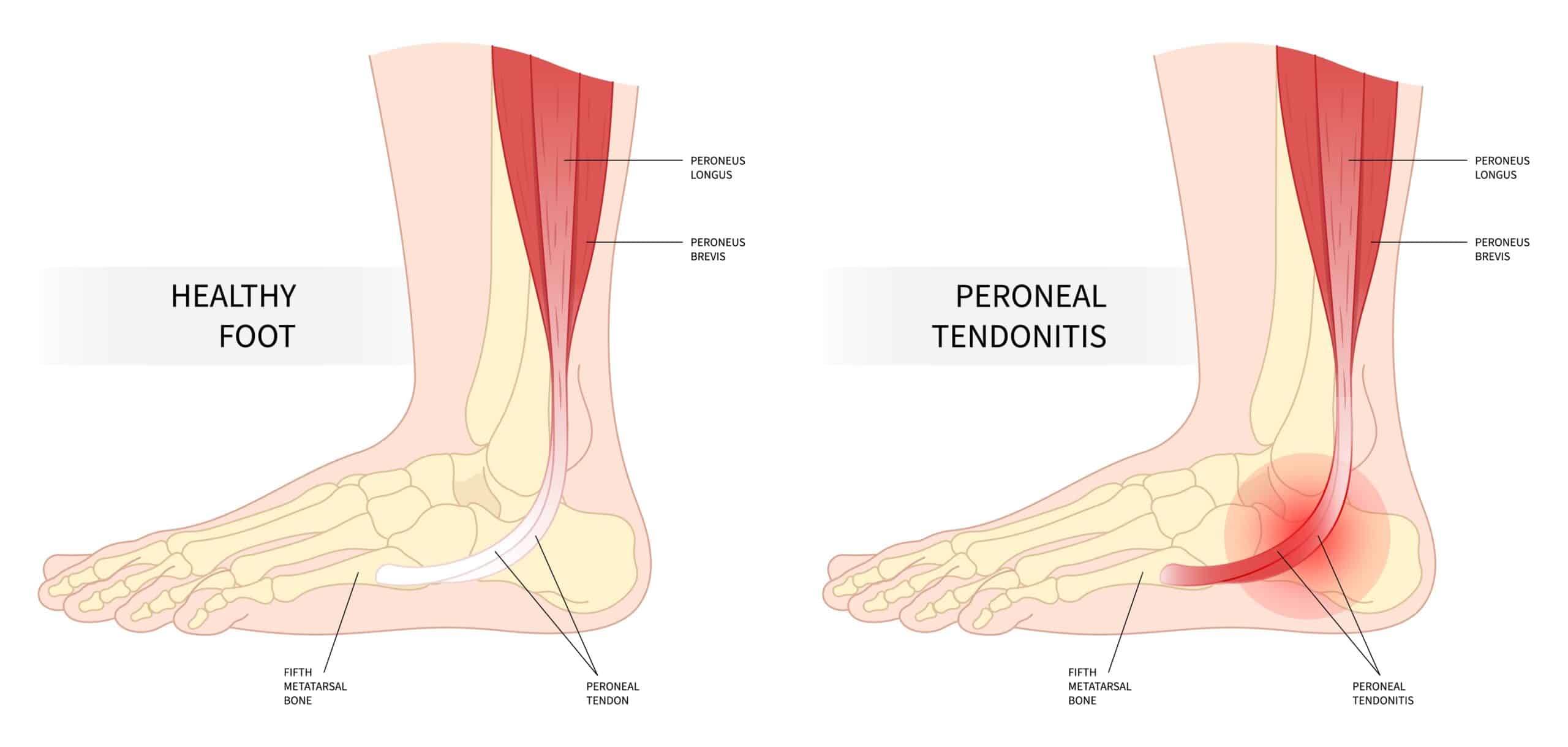
Peroneal Tendonitis (Peroneal Tendinopathy) is characterized by inflammation and degeneration of the peroneal tendons due to overuse, trauma or biomechanical issues. So, let’s look at the Peroneal Tendons in more detail.
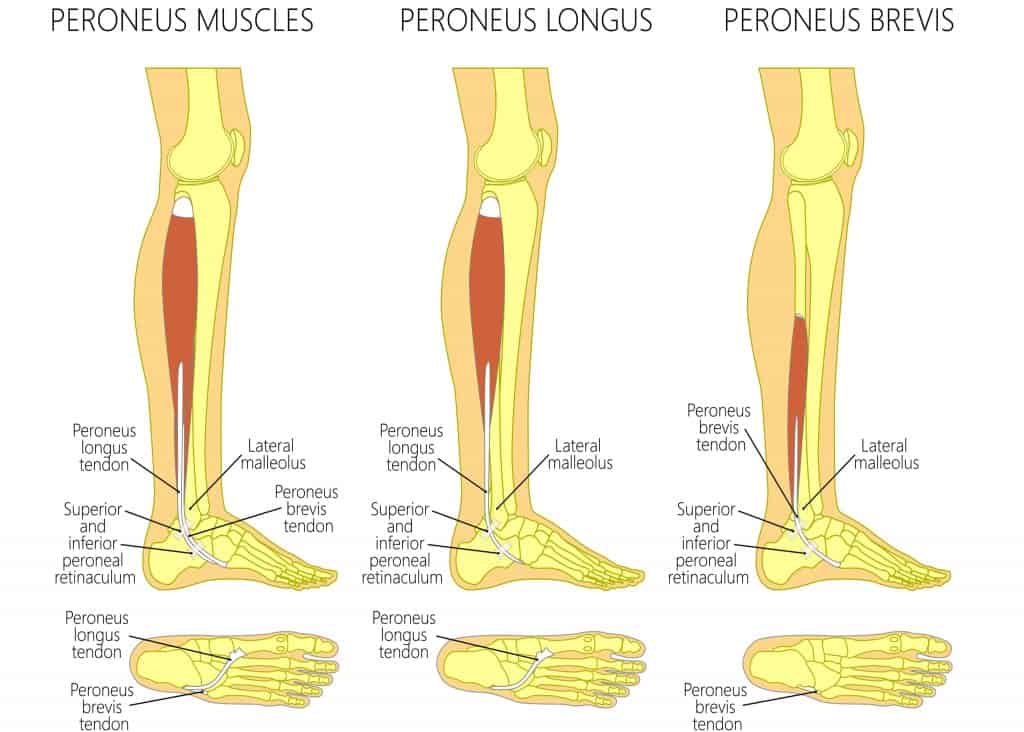
There are 3 main peroneal tendons, the Peroneus Longus, Peroneus Brevis and Peroneus Tertius, although approximately 21% of the population have a 4th peroneus muscle called the Peroneus Quartus.
The Peroneus Longus (fibularis longus) originates from the superior two-thirds of the lateral fibular shaft, anterior and posterior crural intermuscular septa and occasionally from the lateral condyle of the tibia and attaches to the lateral base of the first metatarsal and the medial cuneiform. The main function of the Peroneus Longus is to evert and plantarflex the foot while it helps to stabilise the 1st ray in weight bearing.
The Peroneus Brevis (fibularis brevis) originates from distal two-thirds of the lateral fibula, passes downwards, and loops posterior to the lateral malleolus to insert onto the styloid process at the proximal end of the 5th metatarsal. The function of the Peroneus Brevis is to evert the foot and assists with plantarflexion alongside the Peroneus Longus.
The Peroneus Tertius (fibularis tertius) is present in 42-100% of individuals. Its origin is the distal half or third of the fibula, inserting onto the dorsal surface of the base of the 5th metatarsal. The function of Peroneus Tertius is to assist with dorsiflexion and eversion.
Related Article: Anatomy and Function of the Ankle Tendons
Symptoms
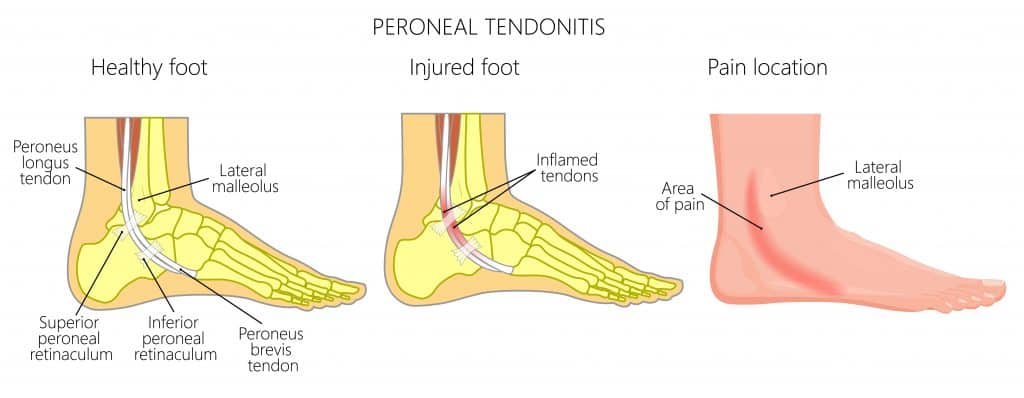
In the acute phase of pain (0-72 hours), Peroneal Tendonitis can cause constant pain on the outer side of the ankle and foot that is painful when walking or turning the foot outwards.
There may be a clicking noise or crepitus along the line of the tendon when moving the ankle and there may be some swelling on the outer ankle.
The most common symptoms of Peroneal Tendonitis in the sub-acute phase are slow and gradual in onset. Patients describe feeling a dull ache on the outer ankle around the lateral malleolus that is stiff in the morning, worse at the start and end of exercise such as a run but the pain improves during the run.
The location of the pain is on the outside of the ankle in the groove just behind the lateral malleolus and onto the foot’s outer side when the peroneal tendons attach to the fifth metatarsal.
If the Peroneal Longus Tendon is inflamed, there may be pain on the foot’s underside.
Walking on uneven surfaces, wearing unsupportive footwear or carrying out impact activities are likely to worsen Peroneal Tendonitis symptoms.
Causes
A repetitive overload of the Peroneal Tendons can cause Peroneal Tendonitis. When running or walking, poor biomechanics can overload the lateral ankle leading to overuse of the Peroneal Tendons. This overuse causes inflammation, irritation, and pathological changes within the tendons, leading to Tendonitis.
A rigid high arch foot can place excess pressure on the Peroneal Tendons and make them more susceptible to overload.
Repetitive ankle sprains can result in Peroneal Tendonitis. The lateral ligaments become stretched, leading to instability of the ankle. The Peroneal muscles compensate by working harder to provide additional stability to an ankle, causing an overload.
Alternatively, an acute ankle sprain can overstretch the Peroneal Tendons, leading to inflammation and tendonitis.
Flat feet and adult-acquired flat feet can lead to excessive foot movement when walking or running, overloading the Peroneal Tendons and causing Tendonitis.
Other causes include poor footwear, sudden increases in walking or running, foot deformities, and hypermobility.

Peroneal Tendonitis Diagnosis
It is essential to see a medical professional, such as a Physical Therapist, for a clinical diagnosis of your pain. After collating your medical history and onset of symptoms, they will carry out a physical examination. A clinical test for Peroneal Tendonitis requires the patient to dorsiflex and evert the foot against the resistance of the practitioner’s hand. A positive test provokes pain in the Peroneal tendons.
Clinicians should assess the stability of the ankle ligaments as part of the assessment while there is normally pain on palpation of the Peroneal Tendons.
An X-ray is a valuable form of imaging to rule out other potential causes of lateral ankle pain, such as osteoarthritis. Still, it cannot be used to diagnose Peroneal Tendonitis correctly. MRI and Ultrasound are the most accurate forms of imaging to diagnose Peroneal Tendonitis clinically, and the results should be correlated alongside a clinical assessment.
There are several conditions that present with similar symptoms to Peroneal Tendonitis on the outside of the ankle and foot, such as:
- Peroneal Nerve Entrapment
- Peroneal Tendon Tear
- Peroneal Tendon Subluxation
- Lateral Malleolus Fracture
- Cuboid Fracture
- Cuboid Syndrome
Peroneal Tendonitis Treatments
Home Treatment
Modifying your activity levels is an important part of managing Peroneal Tendonitis. It is important to avoid resting completely as this can cause deconditioning of the tendon and make it hard to return to previous activity levels.
Consider reducing your activity levels by 20-30% so that your pain becomes more stable with carrying out more non-impact activities.
Applying ice to the Peroneal tendons can reduce your pain levels, and we recommend doing this for 10-15 minutes at a time, 2-3 times daily.
Foam rolling the calf and Peroneal muscles can help relax the muscles and relieve pain, but you should avoid applying direct compression to the tendon.
In the acute phase, it is worthwhile considering taking some anti-inflammatories such as ibuprofen, but you should consult your GP beforehand.
Physical Therapy
Strengthening Exercises are a fundamental aspect of treatment for Peroneal Tendonitis. It is essential to condition the Peroneal Tendon to absorb load from impact activities such as running, walking, and jumping. A tendon can become tight, inflamed, and painful when fatigued.
Strength training, therefore, plays a significant role in increasing the tendon’s capacity, alleviating pain, and reducing the risk of recurrence. As a tendon becomes fatigued, the muscles attaching to the tendon can become tight, leading to further irritation and discomfort. Peroneal stretching can help reduce this tension and provide symptomatic pain relief.
Peroneal Tendonitis Taping involves applying a rigid taping to the ankle can help reduce Peroneal Tendon pain levels as it shortens the tendon. As a result, it doesn’t have to work as hard. Therapist may do this by applying a simple heel lock in a neutral position, while KT Tape has been shown to have minimal to no effect on Peroneal Tendonitis.
Peroneal Tendonitis Brace has a similar role to rigid ankle taping as it reduces movement at the ankle’s subtalar joint. As a result, the Peroneal Tendons don’t have to work as hard to stabilise the tendon. The benefit of a brace over taping is that it is a more permanent fixture, while the downside is it can be obtrusive.
Dry needling can be an effective form of treatment for pain relief, but it does not address the cause of the issue. At the same time, Peroneal Tendonitis Insoles are recommended for individuals who have poor ankle stability. These can be worth trying from off the shelf, and if they are not helpful, it can be valuable to have a gait analysis. The results of a gait analysis by a foot specialist allow them to create custom insoles tailored to your foot’s specific needs.
Other Treatment Options
There can be enough rationale for a steroid injection in very irritable cases of Peroneal Tendonitis. A Sports Medicine Doctor usually carries this out, and it is an ultrasound-guided injection. The benefit includes reductions in pain and inflammation levels. However, there is some evidence that it may contribute to the degeneration of the tendon over time.
A walking boot may be recommended for highly irritable cases for 1-2 weeks, which decreases pain levels, or they are recommended post-injection to allow the steroid to take full effect.
Surgery for Peroneal Tendonitis surgery is rare. The most common type of surgery performed by a Foot & Ankle Orthopaedic Consultant for this is a Peroneal tendon debridement. When recommended, this is generally for very painful tendonitis that has failed all other forms of treatment. It is usually followed by 8-12 weeks of Physical Therapy.
Recovery Time?
Peroneal Tendonitis requires 8-12 weeks of recovery time under the guidance of a Physical Therapist.
If you quickly identify the symptoms of Peroneal Tendonitis and follow the appropriate treatment, then you may recover from the condition within 8 weeks.
In chronic cases of Peroneal Tendonitis, it takes up to 12 weeks to heal after a thorough rehabilitation protocol that addresses any strength deficits and biomechanical issues.
Physiotherapy with James McCormack
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Peroneal Tendonitis.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.