Extensor Tendonitis: Foot
Read More >
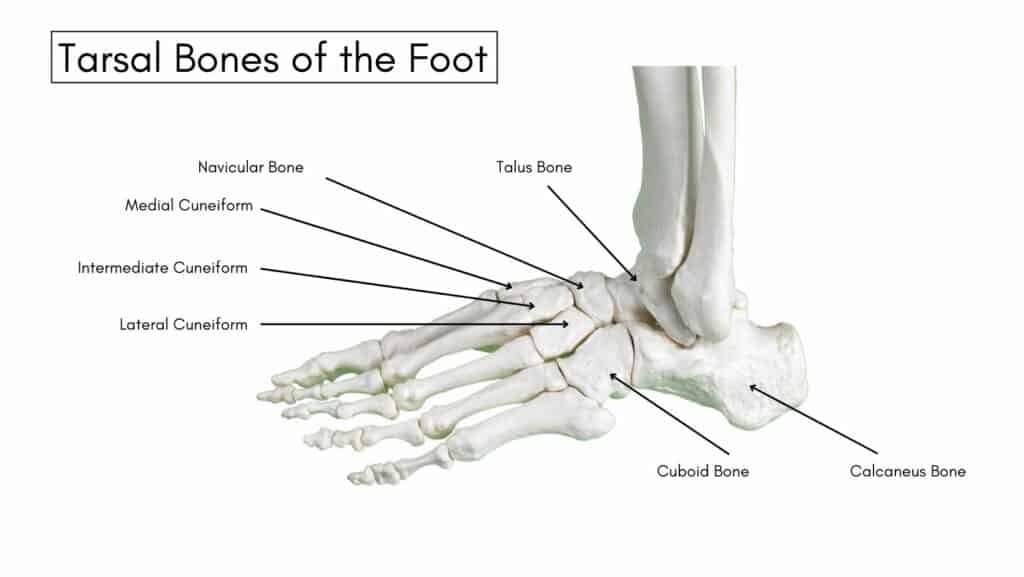
The tarsal bones comprise the back of your foot: the Calcaneus, Talus, Cuboid, Navicular and Cuneiform bones. A Tarsal Coalition is an abnormality in developing one or more tarsal joints.
A study of 574 children over the age of 12 who had an MRI for various reasons identified the prevalence of a tarsal coalition in 11.5% of scans. In contrast, another study of 114 feet of 62 cadavers found a prevalence of 13%, while tarsal coalitions are present bilaterally in up to 50% of cases.
Tarsal Coalitions most commonly affect the calcaneonavicular joint and the talocalcaneal joint; these two joints account for 90% of all cases of tarsal coalition. The tissue that connects these joints to form a tarsal coalition can be completely or partially ossified (synostosis) or consist of cartilage (synchondrosis) or fibrous tissue (syndesmosis).
The symptoms of a Tarsal Coalition most commonly begin in the second decade of life after the joint becomes ossified, although some patients have no symptoms until adulthood.
In individuals with bilateral tarsal coalitions, it is common for ossification to occur at different times, which leads to the asynchronous onset of symptoms.
Pain during physical activity at the coalition’s site is the key symptom of a Tarsal Coalition; a talocalcaneal coalition causes pain under the medial malleolus, and a calcaneonavicular coalition causes dorsolateral pain over the affected site.
Symptoms include pain and stiffness in the hindfoot when walking or doing impact activities such as running or jumping.
Patients often present to the clinic in the second decade due to repetitive ankle sprains that result from restricted mobility to the hindfoot
In children, it is common to see them limping, and often, the pain discourages them from participating in sports.

A significant genetic element to developing a Tarsal Coalition is that the bones develop improperly during fetal development.
Risk factors for Tarsal Coalition include hypoplasia syndromes such as fibular hemimelia, congenital short femur, and proximal femoral focal deficiency.
Tarsal Coalition in adults usually results from arthritis, trauma or infection.
The time from the onset of symptoms from a Tarsal Coalition ranges from 12-18 months.
Tarsal Coalition can be identified as a possible cause of pain by a Physical Therapist or a Sports Doctor following a Physical examination.
Clinical features of a talocalcaneal coalition include the restricted motion of the sub-talar joint. In contrast, patients with calcaneonavicular coalition usually have little or no loss of mobility, as the synostosis does not affect motion at the sub-talar joint.
In the talocalcaneal coalition, the double medial malleolus sign is produced by the widened middle calcaneal facet that is palpable under the medial malleolus.
While an X-ray can identify a tarsal coalition, a CT scan or MRI are preferred as one coalition may hide another.

Conservative treatment is the first treatment option for a tarsal coalition, with a study including 31 feet treated non-operatively and a 5-year follow-up identified 74% of cases were painless and 71% had normal range of motion.
A Physical Therapist provides treatment for a Tarsal Coalition following an assessment of the mobility and strength of the foot and ankle. A gait analysis can identify the need for insoles to provide extra support or the correct type of footwear for the patient.
A rehabilitation protocol consisting of various balance, strength and stability exercises is highly effective.
A period of modified rest from impact activity can be beneficial. In contrast, non-impact activities such as swimming and cycling can temporarily replace impact exercise to allow inflammation levels in the hindfoot to subside.
In some cases, a steroid injection is required to reduce inflammation levels, but this is generally avoided unless necessary in most paediatric cases.
Surgery is the last resort for this condition which can be in the form of joint resection or a joint fusion. There are risks involved with all forms of surgery, and this should be discussed in detail with your Orthopaedic Consultant.
This is not medical advice, and we recommend a consultation with a medical professional such as James McCormack before trying any of these exercises. James offers Online Physiotherapy Appointments weekly.