Peroneal Tendonitis Brace
Read More >
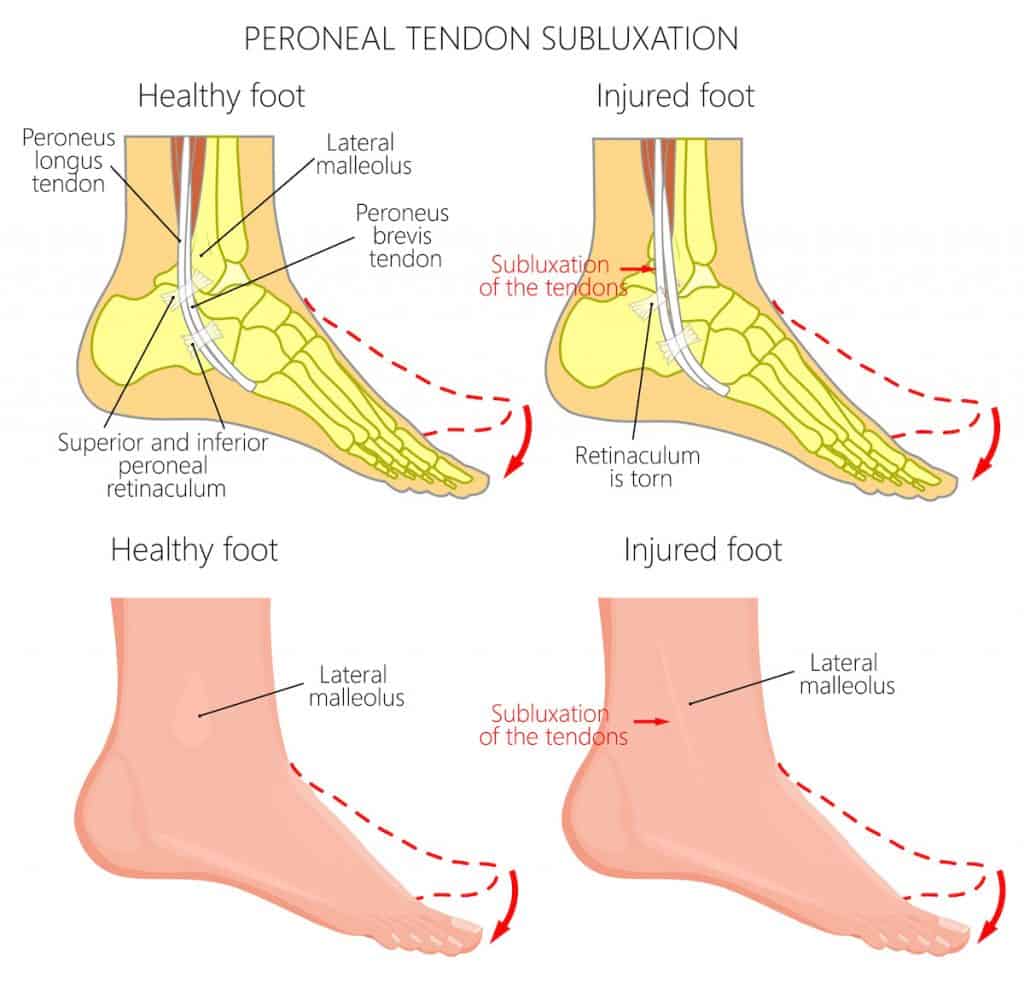
Peroneal Tendon Subluxation is the displacement of the Peroneal Muscles from the deep groove behind the lateral malleolus due to a Superior Retinaculam tear or rupture.
The Peroneal muscles sit on the outside of the shin bone, connecting to the outer and underside of the foot via the Peroneal Tendons. Their function is to turn the foot outwards, assist with plantarflexion and help to stabilise the ankle through gait.
There are 3 Peroneus muscles; Peroneus Brevis, Peroneus Tertius and Peroneus Longus. Peroneus Brevis and Peroneus Longus pass through a groove underneath the lateral ankle bone before connecting to the foot. They are held in the grove, but a strong fibrous band of tissue called the Superior Peroneal Retinaculum (SPR).
Injury to the SPR can allow extra movement of the Peroneus muscles in the grove, allowing them to subluxate from the grove with certain movements. When this occurs, it is known as Peroneal Tendon Subluxation.

When turning their foot outwards, patients often report a loud clicking or cracking noise in their ankles. They may feel pain on the outside of their ankle, and it may be possible to visibly see the tendon popping in and out of its groove.
There may be some swelling on the ankle with pain when turning the foot out, walking, running or changing direction.
Ankle range of movement may be limited due to pain levels and there may be tenderness on palpation of the tendons. In some cases, where there is no retinaculum, they may not feel any pain during or after a subluxation.
Peroneal Tendon Subluxation (PTS) is caused by repetitive lateral ankle sprains that lead to stretching of the Superior Retinaculum (SPR). In contrast, a significant ankle sprain can lead to a complete tear of the SPR. When the SPR is stretched, the peroneal tendons can move out of the groove behind the fibula.
In hyper-mobile individuals, there may not be a specific mechanism of injury, but the SPR is not as rigid as it needs to be. With the contraction of the Peroneal muscles, they push past the SPR and subluxate. In some rare cases, there is no SPR present.
Some patients may also have a shallow groove which increases their risk of subluxation.
Peroneal Tendon Subluxation is more common in dancers, change of directions sports and individuals with hypermobility conditions such as Ehlers-Danlos Syndrome.

Peroneal Tendon Subluxation can be clinically diagnosed by a Physical Therapist or a Sports Medicine Doctor following a clinical examination. A clinical test for Peroneal Tendon Subluxation by a foot specialist involves positioning the patient seated with their knee bent. The clinician places their thumb over the SPR and asks the patient to evert and dorsiflex their foot forcibly. The clinician will feel the peroneal tendon subluxate, sometimes alongside an audible click or pop. The patient may feel pain when this occurs.
The patient may be referred for a scan to confirm the diagnosis and to see if the SPR remains intact. An x-ray is not beneficial in this instance. An MRI is useful for detecting a ruptured or torn retinaculum, but they are expensive and can be challenging to attain.
An ultrasound scan is the most sensitive (100%) and specific (90%) form of imaging for Peroneal Tendon subluxation as it can provide real-time feedback and is dynamic, allowing the patient to subluxate the tendon during the scan.

The Oden Classification describes the different types of subluxations of the Peroneal Tendons.
Grade 1: The Superior Retinaculum (SPR) is pulled from the lateral malleolus
Grade 2: The fibrous ring alongside the SPR is puller from the lateral malleolus
Grade 3: the SPR, fibrous ring and a bony fragment from an avulsion fracture are pulled from the lateral malleolus
Grade 4: The posterior SPR is completely torn
If a Peroneal tendon subluxation occurs with pain, it is advised to seek conservative treatment under a Physical Therapist’s guidance. In the non-athlete population, a patient should try conservative treatment initially but be informed in advance that there is a 50% chance of reoccurrence, according to a study by Ziai et al.
Treatment from a Physical Therapist should consist of Peroneal strengthening exercises, foot and ankle stability, and proprioception exercises.
Peroneal tendon taping with rigid may be used to provide additional stability to the ankle joint, but it’s unlikely to stop the subluxation completely. There is minimal evidence to support using KT Tape for Peroneal Tendon Subluxation.
An ankle brace is an effective treatment for Peroneal Tendon subluxation as it has the same effect as rigid taping and provides better long-term support.
Reducing exercise levels is recommended with some non-steroidal anti-inflammatories such as ibuprofen, followed by a graduated return to sport.
If these methods fail to reduce symptoms, a steroid injection may be carried out to the tendon sheath; this is usually ultrasound-guided. Generally, injections to the tendon are not recommended as they can cause long-term harm to the tendon.
Split tears of the Peroneus Brevis or Longus are common complications of Peroneal Tendon Subluxation, and we have covered this in-depth in a separate article.
Finally, we have separate articles on FAQ’s for Peroneal Tendon pain and articles on what sports or exercises you can do with Peroneal Tendon pain.

Surgery for Peroneal Tendon Subluxation is highly successful. Usually, it consists of a graft to replace the superior retinaculum, or if it is viable, a repair of the superior or posterior retinaculum may be carried out. This is typically followed by a period in a walker boot and 4-6 weeks of physical therapy.
A repair or a reconstruction can include deepening the groove where the Peroneal Tendons sit to reduce the risk of their subluxation in the future.
Post-surgery, the foot is usually placed in a short boot with the foot slightly inverted, and the patient is non-weight bearing for the first 2 weeks. Following this, they are placed in a walker boot for 4 weeks with a gradual increase in weight-bearing activities.
After 6 weeks, the patient can wean out from the boot and commence Physical Therapy. Total recovery time from Peroneal Tendon Subluxation Surgery is 4-6 months.
Peroneal Tendon Subluxation with no pain?
There is no need for treatment when there is a subluxation of the peroneal tendon without pain. There may be a lax superior retinaculum or none at all, but asymptomatic subluxation of the tendon is harmless.
Can Peroneal Tendon Subluxation heal on its own?
You don't need any treatment if you have a Peroneal Tendon Subluxation with no pain. If you have a Peroneal Tendon subluxation that is increasingly painful, it is unlikely to heal on its own, and we recommend that you see a Physical Therapist for treatment.
Do I need surgery for Peroneal Tendon Subluxation?
If you have pain and have tried conservative treatment without success, you are a candidate for Peroneal Tendon Subluxation Surgery. This is a highly successful treatment, and it is unlikely to recur. If you have no pain, then you do not need surgery.
Peroneal Tendon Subluxation after Ankle Sprain
It is possible to develop a Peroneal Tendon subluxation after an ankle sprain. This often occurs with a high-grade lateral ankle sprain as the Peroneal tendon, and superior retinaculum can become overstretched or tear. If this occurs, it can allow the Peroneal Tendons to subluxate and be misdiagnosed as an irritable chronic ankle sprain or Peroneal Tendonitis.
This is not medical advice, and we recommend a consultation with a medical professional such as James McCormack to achieve a diagnosis. He offers Online Physiotherapy Appointments.
Other causes of Peroneal Tendon Pain
Peroneal Tendonitis
Peroneal Tendon Tear
Superficial Peroneal Nerve Pain