Plantar Fasciitis Insoles & Inserts
Read More >
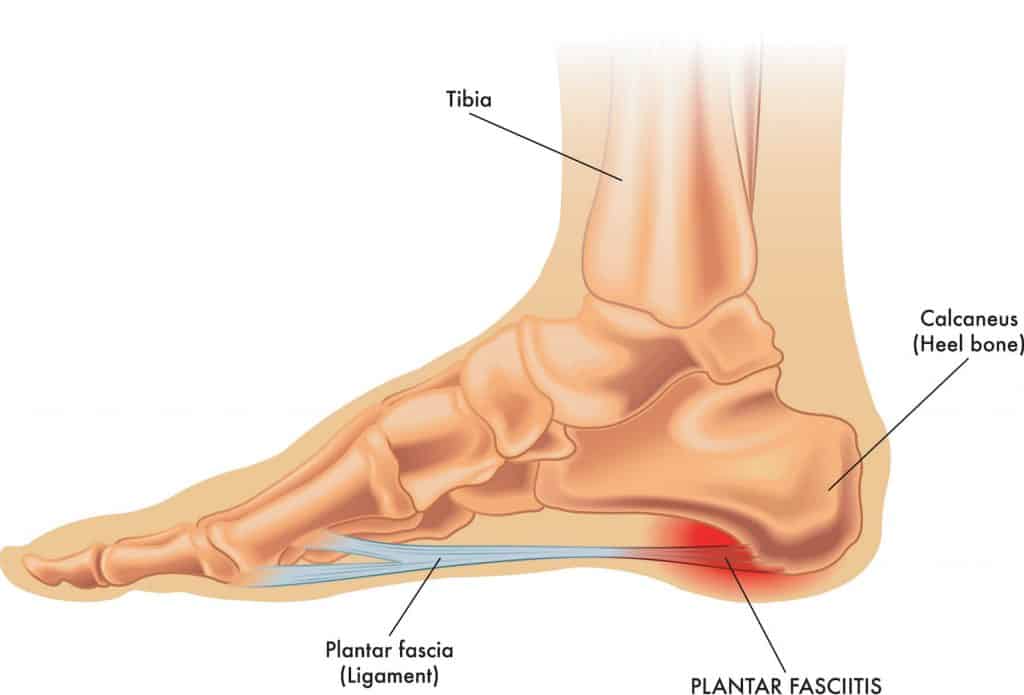
The Plantar Fascia is a thick, fibrous band of connective tissue on the underside of your foot. The origin of the Plantar Fascia is the inner (medial) side of the heel bone and spreads out like a fan to attach across the underside of the forefoot.
The Plantar Fascia is a passive structure, so unlike a muscle, it cannot actively contract. It provides stability to the medial arch of the foot which means that it is under constant tension in a standing position.
Another vital function of the Plantar Fascia is its role in the windlass mechanism. As the toes are extended, it places tension on the Plantar Fascia, which acts as a stabiliser on the foot’s arch. This is a critical function in the push-off phase of the gait cycle.
It is one of the most prevalent conditions of the lower limb affecting 10% of runners, and 11-15% of all foot conditions.
The plantar fascia is a non-contractile tissue. Unlike a muscle, its primary function is to provide stability to the underside of the foot and the medial longitudinal arch (MLA).
When walking, running, or hopping the plantar fascia absorbs force and stabilises the foot.
If the Plantar Fascia becomes overstretched or irritated from overuse or through an overload, such as a sudden change in activity levels, it can result in inflammation and pain of the Plantar Fascia.
Risk Factors
Plantar Fasciitis is most often associated with pain in the inner aspect of the heel bone (Calcaneus) during weight-bearing activities such as standing, walking, hiking, or running. This pain may extend into the arch of the foot. This non-insertional plantar fascitis should not be confused with Posterior Tibial Tendonitis.
The most common symptoms are pain and stiffness in the morning when stepping out of bed. This generally eases after 5-10 minutes of walking, but this pain may persist for longer in more severe cases. A similar sensation may occur when standing and walking after sitting for an extended period.
Plantar Fascia pain is associated with movement and is often worse at the start of an activity such as walking or running but as circulation increases in the area through activity, pain levels may decrease before returning in the hours after exercises. As symptoms deteriorate in more chronic cases, pain may not ease but get gradually worse.
Pain should subside in non-weight-bearing positions. If it doesn’t and the pain keeps someone up at night, it is important to consider what other conditions may be causing similar symptoms to Plantar Fasciitis.

A diagnosis of Plantar Fasciitis is achievable through a consultation with a medical professional.
A clinical examination of the foot position, gait, strength, and mobility of the entire lower limb should follow this. The therapist will apply pressure to the medial aspect of the calcaneus, and if this is painful, then the likelihood is high that Plantar Fasciitis is present.
Clinical tests should be carried out to rule out all other conditions that can cause similar symptoms, such as a calcaneus stress fracture.
Imaging can be helpful to confirm the diagnosis. High-frequency ultrasound is useful to identify any thickening of the Plantar fascia along with any inflammatory signals.
An MRI may be requested to provide a more in-depth picture of the plantar fascia and the surrounding areas of the foot and ankle.

Treatment under the guidance of a Physical Therapist is highly recommended for this condition as it is complex to manage and requires a combination of different treatment strategies to recover from Plantar Fasciitis. In this section, we are going to explore the various treatment methods currently available to us.

Off-the-shelf insoles are effective at reducing pain levels in Plantar Fasciitis. Lee et al, 2012, found that using insoles alongside night splints provided more pain relief than either on their own.
Self-massage tools such as a tennis ball, foam roller, massage gun or socks can provide immediate relief but are often temporary.
A tens machine provides effective pain relief, and Voltaren gel is a good localised anti-inflammatory. Still, it is essential to let it dry entirely before covering the foot with clothing.
An excellent review was published in 2021 highlighting the importance of education, taping and stretches for treating Plantar Heel Pain.
For moderate to severe symptoms of Plantar Fasciitis, it can be too painful to walk, let alone carry out strengthening exercises. In these instances, the following modalities can help reduce pain levels:
A silicone heel cup can provide pain relief to the heel, especially for those who spend a lot of time standing throughout the day.
There is strong evidence to support the use of Plantar fasciitis taping. It can reduce pain levels to facilitate rehabilitation and is performed using zinc oxide tape.
We have created a video to guide you on self-taping for heel pain.


Strengthening Exercises normally form a key part of treatment. It helps by conditioning the Calf Muscles and Plantar Fascia to tolerate more force when exercising.
These should become progressively difficult through adding more weight and may then progress into a plyometric program.
Plantar Fasciitis stretches should form a key part of a comprehensive rehabilitation protocol and you can find some later in the article.
A Gait Analysis and running gait analysis are beneficial to identify biomechanical issues that may be causing an overload of the Plantar Fascia.
Some cases may benefit from custom insoles, or prefabricated ones may be sufficient.
Extracorpeal shock wave is a form of treatment that has been demonstrated to be moderately effective for Plantar Fasciitis. It can be used alongside strengthening exercises.
By sending acoustic waves through the tissue it is believed to have an effect on sensory fibres leading to an analgesic effect.
There is minimal downside to having this treatment with evidence highlighting no side effects.


Steroid Injections have demonstrated good effects in reducing pain levels in Plantar Fasciitis.
Its effectiveness appears to last for 1 month on average. However, it increases the risk of Plantar Fascia rupture and/or fat pad atrophy.
To reduce these risks, an experienced physician should perform an ultrasound-guided injection.
There is some emerging evidence to suggest that PRP is as effective in providing pain relief as a steroid injection for Plantar Fasciitis but with longer-lasting benefits.
However, we await further studies and public or private healthcare companies rarely cover it.

Plantar Fasciotomy involves the surgical release of 2/3 of the Plantar Fascia. This should be considered a last resort and while there is some positive results we are awaiting high level studies to confirm its effectiveness. It is normally followed by a period of time in a boot before recommencing Physical Therapy.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Plantar Fasciitis.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.