Foot Pain Chart
Read More >
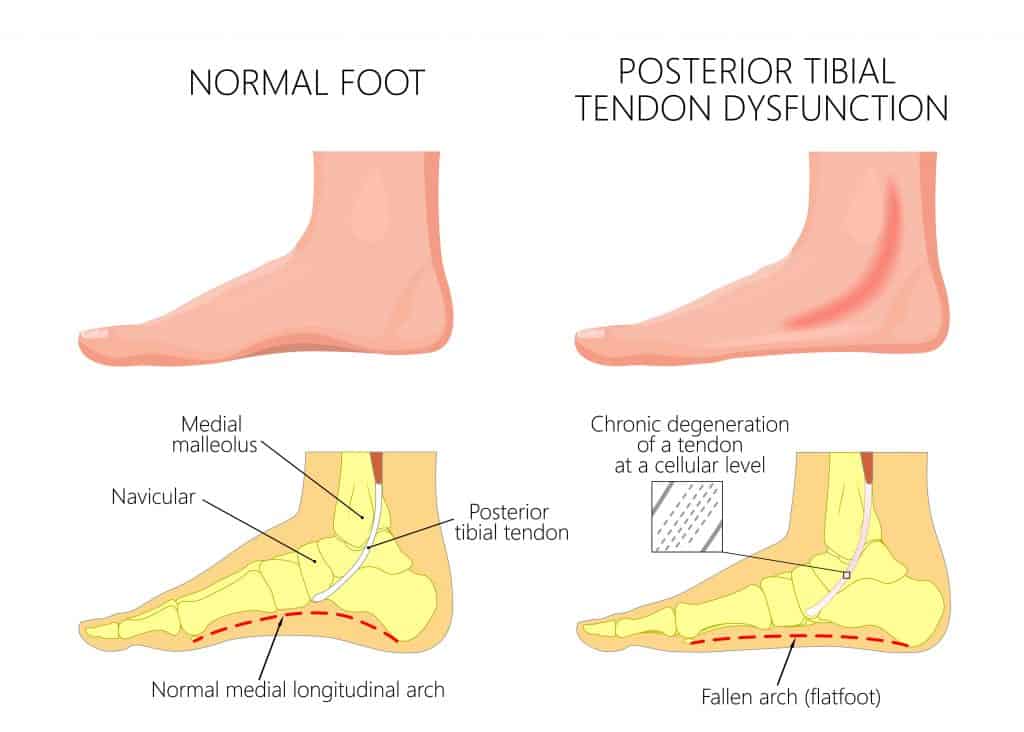
The Posterior Tibial Tendon is a long, thin tendon that runs along the inner ankle. A tendon attaches a muscle to a bone, and the Posterior Tibial Tendon attaches the Posterior tibialis muscle to the side of the foot, mainly the navicular bone.
The Tibialis posterior arises from the interosseous membrane and adjacent surfaces of the proximal tibia and fibula passing down the shin around the posterior aspect of the medial malleolus. The attachment site of the Posterior Tibial Tendon varies anatomically, but the main attachment site is the navicular bone. The second most common attachments are the lateral and medial cuneiforms, metatarsal bases, cuboid, intermediate cuneiform and Calcaneus.
The main action of the Posterior Tibialis is to turn the foot inwards (inversion) and downwards (plantarflexion). When walking, standing, and running, it acts as a key stabiliser of the foot’s medial arch. When the Posterior Tibial Tendon becomes overloaded, it becomes inflamed, irritated and painful, resulting in tendonitis.

In most cases, Posterior Tibial Tendonitis is caused by a change in activity levels. For one person, this may be walking 500-1000 more steps in one day; for another, it could be increasing their weekly running distance from 30 to 60 miles. Sudden changes in running speed, volume, or intensity can play a role.
Ankle Injuries: Ankle sprains can lead to compensatory movements that overload the foot’s medial arch and cause Posterior Tibial Tendonitis. This can also be the case in scenarios where someone is recovering from an ankle fracture.
The ankle joint can become stiff as a result, leading to greater demand on the midfoot through the gait cycle and overloading the Posterior Tibial Tendon.
Foot Type: A flat foot, especially an adult-acquired flat foot secondary to Posterior Tibial Tendon Dysfunction, can lead to tendonitis as excess stress and stretch are placed on the Posterior Tibial Tendon.
Posterior Tibial Tendonitis is less common in those with a high arch, although it is possible in those with a stiff big toe as they struggle to push off.
Related Article: Conditions Causing Inner Ankle Pain
Running: This is one of the most common causes of Posterior Tibial Tendonitis. The action’s high impact and repetitive nature can easily overload the medial foot, especially if there is a sudden change in running volume or speed. We commonly see this in Marathon Training plans. The combination of continued increased running volume alongside interval and hill training can be a significant risk factor for Posterior Tibial Tendonitis.
Barefoot running is not necessarily bad for feet, but evidence suggests that novice runners should have more cushioned shoes, and over time they can reduce levels of support.
Birkenstocks do have the potential to overload the Posterior Tibial Tendon. They are one of the more supportive forms of sandals but not as supportive as trainers.
Finally, being overweight is a risk factor as the extra weight can place more pressure on the medial arch of the foot where the Posterior Tibial Tendon attaches.
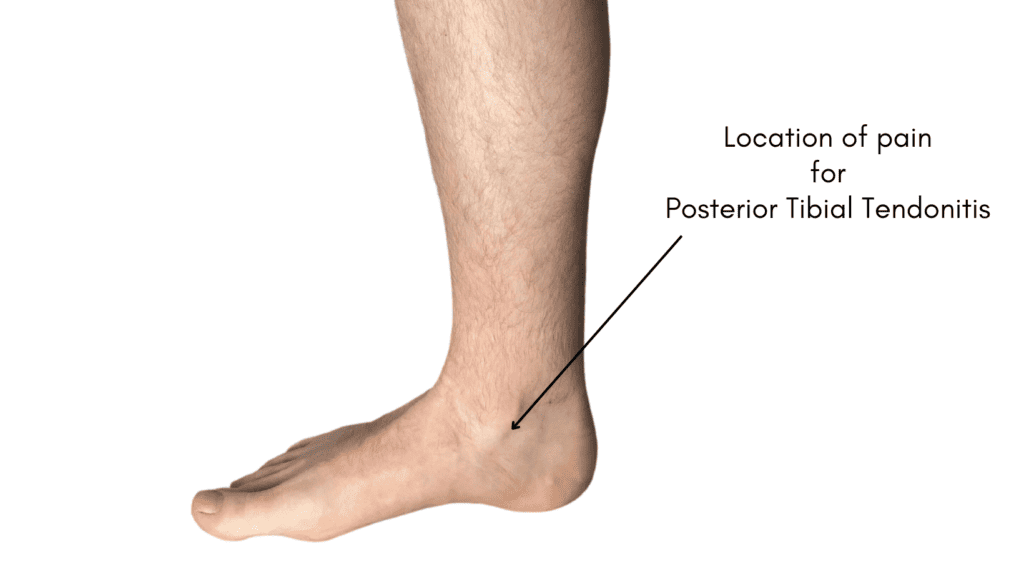
Posterior Tibial Tendonitis (Posterior Tibial Tendinopathy) symptoms are located on the inner ankle as the tendon wraps around the back of the fibula, and pain can extend down onto the insertion of the tendon onto the medial longitudinal arch of the foot. In acute episodes, there may be some visible swelling along the tendon line, but it is unusual to see bruising as this is more indicative of a tendon tear.
The pattern of pain is that the tendon is painful first thing in the morning when stepping out of bed, but this should ease within an hour. Pain is mechanical, meaning that the pain is worse during or immediately after use and should decrease with rest.
If the tendon is aggravated during the day, it may be sore at night when going to bed, but it is uncommon for Posterior Tibial Tendonitis to wake you from your sleep.
In acute episodes, it may be too painful to walk, and there may be a crunching or clicking sensation. The pain is often sharp and becomes more of a dull ache in more chronic cases. In long-term cases, it is not unusual for symptoms to develop in both feet as the previous unaffected side becomes overloaded.
In chronic cases, patients may develop a reduction in the foot’s arch height due to the weakening of the tendon. In severe cases, weakening can lead to Posterior Tibial Tendon dysfunction and an adult-acquired flat foot.

A diagnosis is achieved following a clinical interview, and clinical tests involve palpating the tendon for pain and resisting the movement of plantarflexion and inversion. If there is pain in resistance to this movement, tenderness on palpation of the tendon and pain when hopping, there is a high likelihood that the patient has Posterior Tibial Tendonitis.
Diagnostic ultrasound is recommended for imaging as it has high accuracy and low cost. An MRI is another form of scan that can diagnose Posterior Tibial Tendonitis, but it is more expensive.
An X-ray is useful to rule out conditions that provide symptoms similar to Posterior Tibial Tendonitis, but it’s impossible to diagnose it using an X-ray.
As part of the diagnostic criteria, it is important to rule out other conditions of the inner ankle, especially Flexor Hallucis Longus pain, as it is often misdiagnosed as Posterior Tibial Tendonitis.
It is possible to manage an acute episode of Posterior Tibial Tendonitis at home. If you suspect you have the early symptoms of tendonitis, you could try the following:
Physical Therapy is the best and most evidence-based treatment for Posterior Tibial Tendonitis. It covers an array of forms of treatment, and we will cover the most effective.
Posterior Tibial Tendonitis Taping is an effective way to offload the Posterior Tibial Tendon, helping to reduce pain levels. This usually involves a rigid figure-6 ankle taping to hold the ankle in neutral of 5º of inversion.
At the same time, a Posterior Tibial Tendonitis brace is effective at supporting the ankle and providing pain relief. This is a short to medium-term solution.
Activity modification involves managing time on your feet to facilitate recovery. Usually, with runners, we try to keep them running at a reduced volume. Running can be replaced with non-impact activities.
This helps to facilitate strengthening exercises for Posterior Tibial Tendonitis, the most effective form of treatment for Posterior Tibial Tendonitis.
These usually begin as band strengthening, progressing into weight-bearing and hopping exercises.

A Gait Analysis may be required if your therapist feels a biomechanical issue is causing your pain. They might assess your gait using a slow-motion video to identify an overload of the inner ankle. Insoles or Orthotics may be prescribed as these are very effective long-term solutions for pain relief. Supportive footwear can help to offload the tendon and provide pain relief.
Steroid injections such as corticosteroids are effective in providing pain relief for cases struggling to adapt to strengthening exercises. Still, it is to be avoided where possible as they cause long-term deconditioning to the tendon.
1-2 weeks in a walking boot is generally recommended post-injection. Surgery is a last resort for Posterior Tibial Tendonitis. This may involve debridement of the tendon and is usually followed by 12 weeks of Physical Therapy.
Other forms of treatment may include acupuncture for pain relief. Posterior Tibial Tendon night splints have minimal benefit, and compliance is poor as they are uncomfortable to wear.
Related Article: Best Exercises for Posterior Tibial Tendonitis
In our experience, recovering from Posterior Tibial Tendonitis takes 6-12 weeks.
In acute Posterior Tibial Tendonitis, there can be constant and sharp pain in the inner ankle. If symptoms are managed correctly under the guidance of a Physical Therapist with offloading, taping, non-impact exercises, and the appropriate footwear, it can take 6 weeks to recover.
Chronic Posterior Tibial Tendonitis can lead to pain and dysfunction of the ankle joint with secondary injuries. It is essential to see the appropriate treatment from a Physical Therapist involving strengthening exercises, footwear advice, insoles and shockwave therapy to heal Posterior Tibial Tendonitis within 12 weeks from the beginning of your treatment.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Posterior Tibial Tendonitis.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.