Read More >
- Anterior Ankle Impingement - July 24, 2022
- Tarsal Coalition - October 12, 2022
- Sural Nerve Pain - October 3, 2022
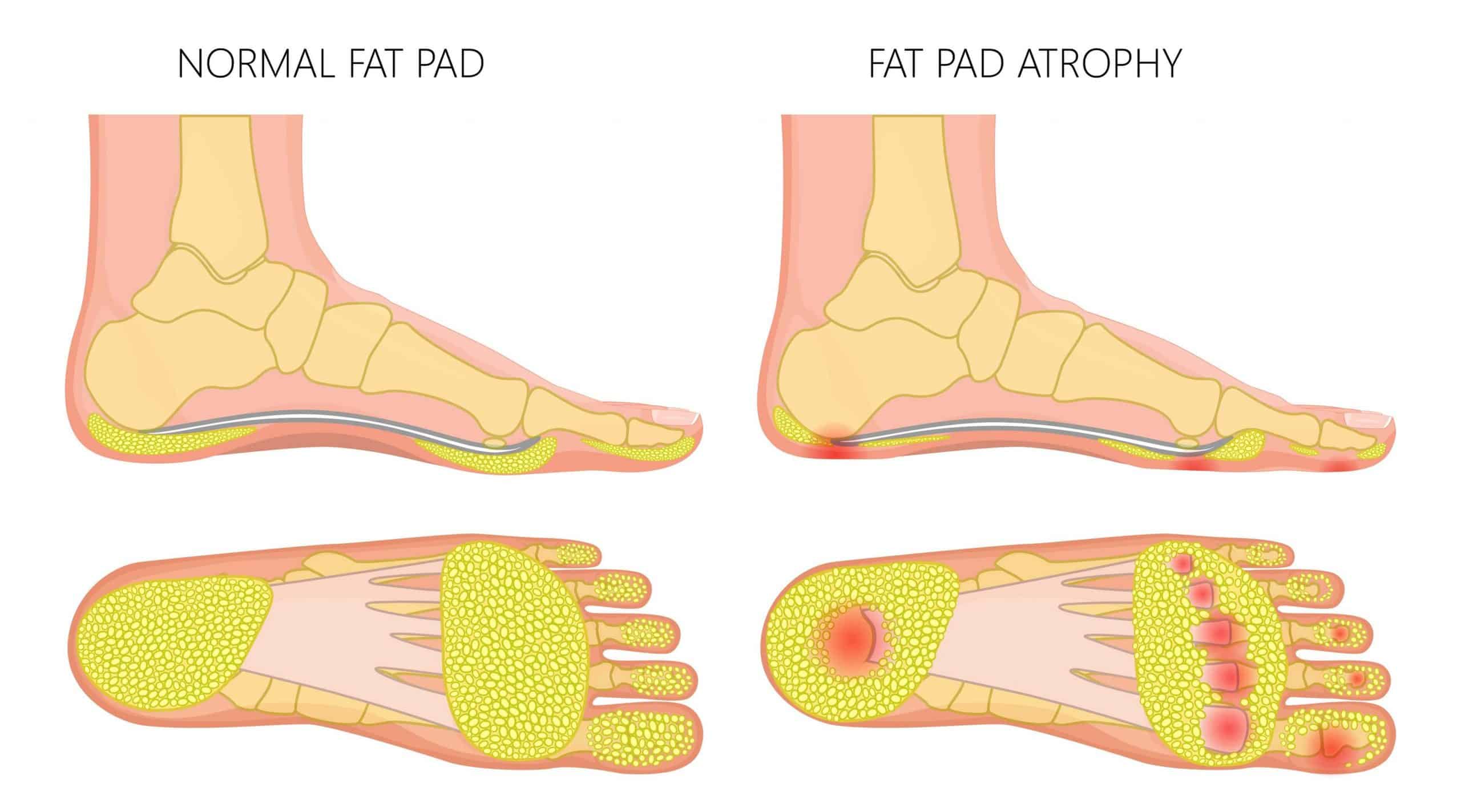
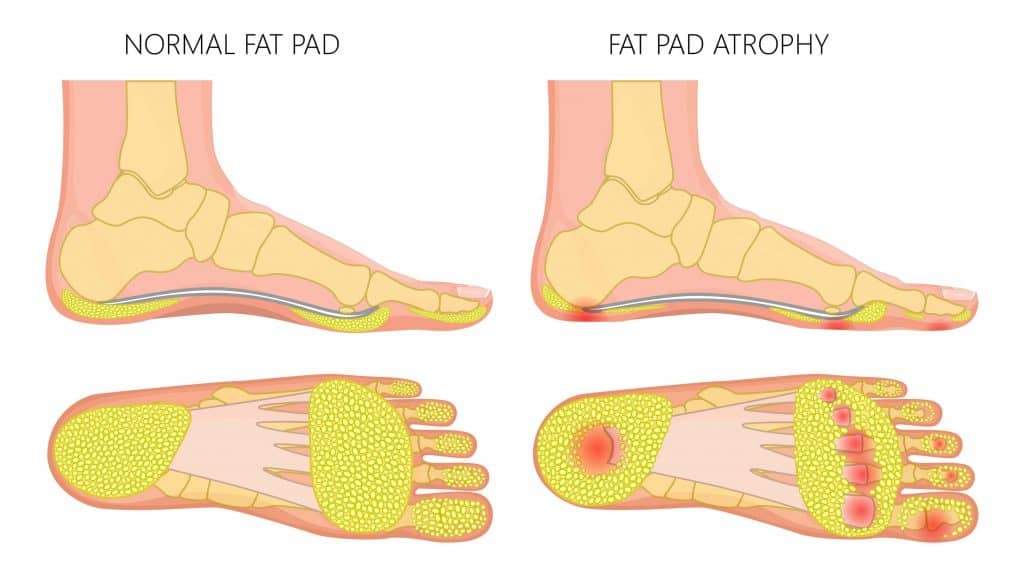
What is the Plantar Fat Pad?
The Plantar Fat Pad of the metatarsals sits on the underside of the foot, under the forefoot. It is a section of fatty tissue that is highly innervated by nerves. Its primary function is to provide cushioning and act as a shock absorber when walking or running while distributing force evenly across the forefoot. The plantar fat pad protects the area’s heel and metatarsal bones and joints with a healthy fat pad typically measuring 1-2 cm in thickness.
This article discusses the causes, symptoms and treatment for Fat Pad Atrophy.
Symptoms of Fat Pad Atrophy
Fat Pad Atrophy symptoms include a thinning of the underside of the forefoot. This may present with more hardened skin or callus, indicating increased pressure on the area.
In severe cases, it can be painful to walk barefoot, and it is often worse when walking on hard surfaces. Patients can feel burning when standing or walking while wearing high heels or heel boots, which often worsens symptoms.
Causes of Fat Pad Atrophy
Several factors influence Fat Pad Atrophy, such as:
- Age
- Family History
- Rheumatoid Arthritis
- Diabetes
- Steroid Injections
- Poor Footwear
- Obesity
Diagnosis
A clinical examination by a Physical Therapist can identify protruding of the metatarsals, and pain on palpation alongside a clinical interview usually is sufficient to develop a diagnosis for Fat Pad Atrophy.
In some cases, a referral for imaging may be required, and an MRI or Ultrasound scan is sufficient to identify changes to the thickness of the fat pad.
We can diagnose Calcaneal Fat Pad Atrophy clinically by comparing left and right heels in weight-bearing and non-weight-bearing positions or through an ultrasound scan.
A normal Calcaneal Fat Pad is 1-2cm thick, but a Fat Pad measuring >1cm can be considered atrophied. An X-ray is rarely used as it cannot diagnose fat pad atrophy.

Treatment for Fat Pad Atrophy
Insoles and Orthotics can be custom-made to provide additional cushioning under the forefoot, reducing the impact on the metatarsal heads.
We recommend full-length insoles so that the cushioning stays underneath the forefoot when walking, as 3/4-length insoles can slide underfoot, causing further irritation.
A cushioned trainer works well, and we recommend the Hoka One running shoe and Sketchers GOWalk shoe for walking as they have a wide toe box, good cushioning, and a flexible toe box which aids the push-off phase of the gait cycle.
Taping can bunch the fatty tissue together to relieve pain, while a sleeve or sock for Fat Pad Atrophy is a cost-effective treatment that cushions the forefoot.
Other Treatment Options for Fat Pad Atrophy
Surgery to graft fat from other anatomical locations such as the abdomen and inject it into the forefoot. There is sufficient evidence to support this procedure for pain relief for up to 2 years.
Physiotherapy with James McCormack
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack. He offers Online Physiotherapy Appointments.
Related Article: Shoes & Insoles for Fat Pad Atrophy
What does Fat Pad Atrophy look like?
Fat Pad Atrophy presents as a thinning of the padding under the forefoot. In severe cases, the metatarsal bones may protrude with severe callus formation under the forefoot.
What does Fat Pad Atrophy feel like?
Patients describe Fat Pad Atrophy as a burning sensation when standing, and when walking barefoot, they can feel like there is no padding under their foot, and it is like they are walking on their bones.
Can fat pads on feet be restored?
Fat Pad grafting for other body parts can be carried out for pain relief in the short to medium term, but it is not a long-term solution. Currently, restoration of fat pads is not possible.