Peroneal Tendon Subluxation
Read More >
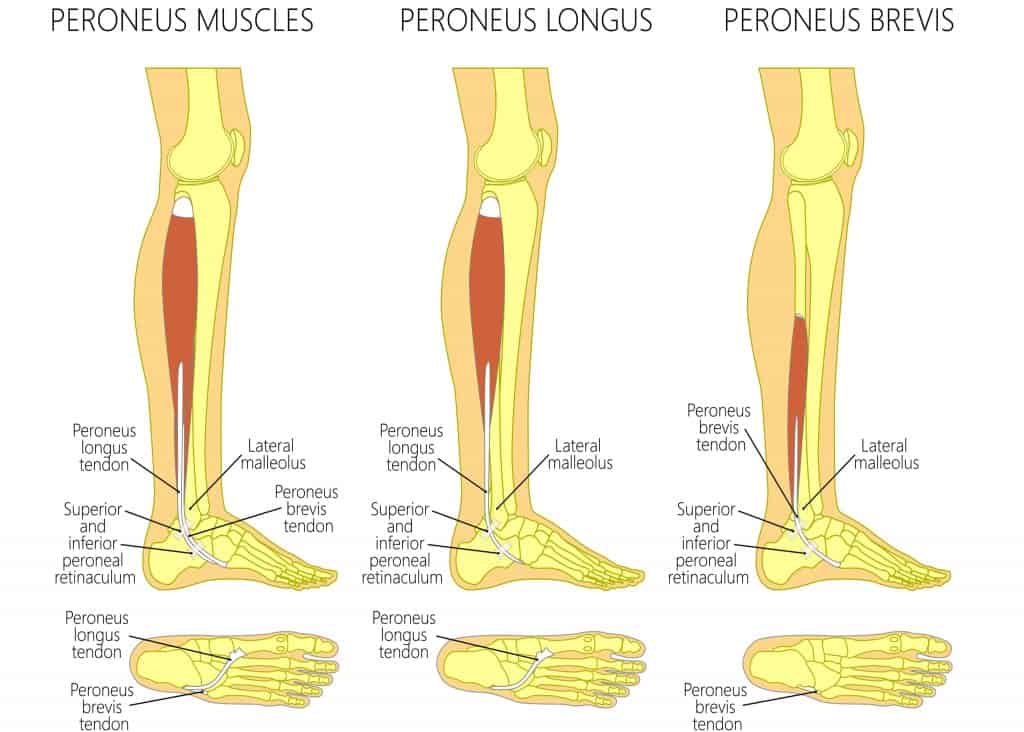
There are 3 Peroneal Tendons on the outside of the ankle, Peroneus Brevis, Tertius, and Longus. Their main function is to provide stability to the foot and ankle through the gait cycle. Due to their anatomy, there is a compression site as they wrap around the head of the fibula bone that can lead to Peroneal tendon tears. The most common of these is a Peroneal Brevis Tendon Tear.
The Peroneal tendons attach from the outer side of the fibula to the outer ankle and underside of the foot. There are three common sites of tears to these tendons. One is as they pass under the ankle bone, leading to pain on the outer ankle when walking or turning the foot outwards. The other less common site is on the outside of the foot as the tendon attaches to the 5th metatarsal and finally on the cuboid tunnel.
Pain is normally sudden in onset for acute tears. A large tear may cause an audible click or popping noise. This is often followed by bruising in the area and a burning type of pain. After the initial injury, symptoms are normally associated with movement, and there is little to no pain at rest.
Degenerative tears often occur in the Peroneal Brevis as it wraps under the fibula. Symptoms are slower in onset and mechanical, making it difficult to differentiate between a degenerative Peroneal Tendon Tear and Peroneal Tendonitis.
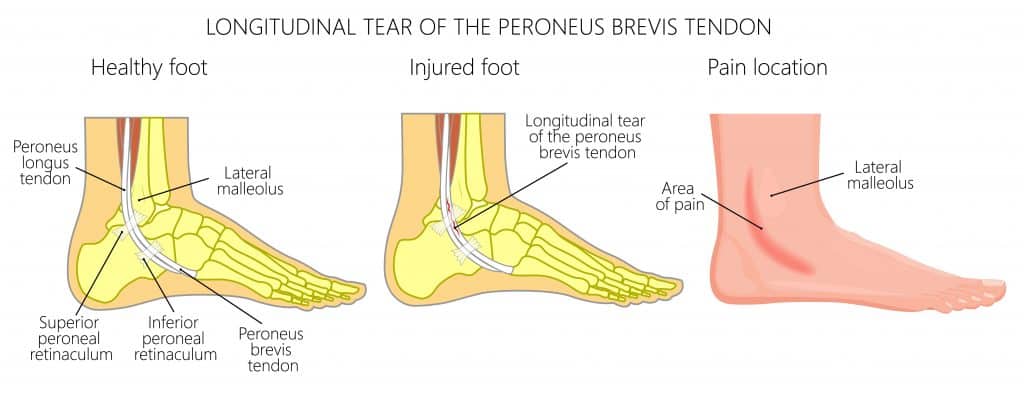
A split tear of the Peroneus Brevis tendon can occur as the tendon wraps around the fibula bone. One of the most common causes of this is ankle sprains that lead to stretching of the Superior Peroneal Retinaculum, allowing the tendon to rub off the sharp posterior edge of the fibula, resulting in a longitudinal split.
This can be hard to detect clinically, especially in an acute ankle sprain. Look for signs of a Peroneal Subluxation and keep it in mind as a differential for chronic ankle sprains with tenderness and swelling on the posterior aspect of the lateral malleolus.
In rare cases, there can be a Peroneus Brevis split without a history of ankle sprains or instability. This case presented with lateral ankle pain, pain on passive inversion and pain on palpation posterior to the tip of the fibula.
The peroneus longus everts and plantarflexes the foot while supplementing lateral ankle stability. The tendon course is long and complex, making two sharp turns at the retro malleolar region and cuboid tunnel before inserting at the medial-plantar forefoot.
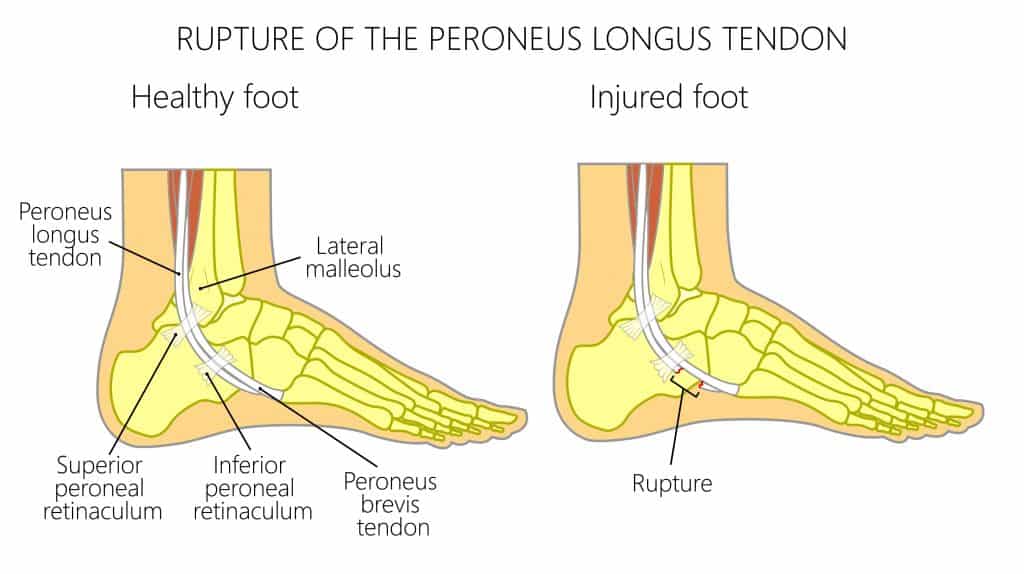
A study by Brandes & Smith found that the cuboid tunnel is the most common site for peroneus longus tears (77%) due to the acute tendon turn at this point and high shear stresses. All complete tears were found in this location.
The precise position of the tendon within the cuboid tunnel varies with foot position. Imaging studies show plantar subluxation of the tendon during dorsiflexion can ease the stress on the tendon. One study demonstrated subluxation in 65% of asymptomatic cases.
For a clinical differential diagnosis, palpate the head of the 5th metatarsal and move proximally into the cuboid tunnel. There is often pain on palpation here without pain on the 5th metatarsal.
These cases are more common in patients with a cavo-varus foot position.
There are two common ways to develop a Peroneal Tendon Tear. The most common is a sudden tear through an acute ankle movement, such as a lateral ankle sprain where the ankle suddenly turns inwards. This movement can overstretch the tendon, causing a horizontal tear or, less often, a longitudinal split of the tendon.
Other causes are often biomechanical, where compression of the tendon over time, particularly the Peroneal Brevis tendon as it gets wedged between the fibula head and the Peroneal Longus, along with a poor blood supply, can lead to a degenerative tear of the tendon.
Peroneal Tendon Tears can be diagnosed in a clinic by a Physical Therapist. A Peroneal Tendon tear test involves the patient lying on their front with their knee flexed to 90º. The therapist resists the foot movement as the patient forcibly dorsiflexes and everts the foot. It is a positive test if this action reproduces pain in the Peroneal tendon.
An MRI is one of the most accurate forms of imaging used to diagnose Peroneal tendon tears. Another useful form of imaging alongside clinical testing is an ultrasound scan, as it can give live imaging and is cost-effective. An X-ray is not a useful tool to diagnose a Peroneal Tendon Tear, although it may be useful to rule out other potential pathologies in the area.
Using these scans, a therapist can provide a diagnostic grading of a Peroneal Tendon tear. These are graded 1, 2, or 3 (high-grade tears) or could indicate the less common longitudinal Peroneal tendon tear. This information is extremely beneficial as it directly impacts recovery times.
If a Peroneal Tendon Tear occurs at the fifth metatarsal, it can be considered an avulsion fracture.
Physical Therapy is the most effective form of treatment for a Peroneal Tendon tear. Following a clinical assessment of the biomechanics, mobility, and strength of the foot a graded strengthening exercise program is developed for the patient.
In the acute phase of injury (0-72 hours), rigid ankle taping can be beneficial to offload the Peroneal Tendons, therefore reducing inflammation and providing pain relief. A longer-term solution for reducing the irritability of symptoms is an ankle brace. KT Tape for Peroneal Tendon Tears has been shown to have little to no benefit for these cases.
If pain levels remain too high to continue rehabilitation, a walking boot may be required for 1-2 weeks before recommencing strengthening exercises.
Injections for Peroneal Tendon tears are not recommended as they can decondition the tendon’s health, while there is mixed evidence for the benefit of other injections such as PRP.
Surgery for a Peroneal Tendon tear is often the last resort for non-resolving grade 1-2 tendon tears, while a grade 3 rupture may be repaired by surgery. A longitudinal tear that is painful and unsuccessfully managed with conservative treatment often responds well to surgical repair. The most common is a longitudinal Split tear of the Peroneus Brevis Tendon. Surgery is typically followed by a short period in a walker boot and Physical Therapy for 6-8 weeks.
A low-grade Peroneal Tendon tear can heal on its own without surgery although it will be weaker than before the injury and we recommended seeing a Physical Therapist for structure rehabilitation.
A high-grade Peroneal Tear or longitudinal tear of the Peroneal Tendon may not heal on its own without surgery despite having adequate conservative treatment.
A longitudinal Tear is unlikely to heal on its own and in most cases, they require surgery to recover.
This article is written by James McCormack, a Foot and Ankle Specialist who is an expert in treating Peroneal Tendon Tears.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.