Achilles Paratenonitis
Read More >
Written by:
James McCormack – Lower Limb Specialist with over 10 years of experience treating and helping patients with Knee, Foot and Ankle injuries.
The Achilles Tendon attaches the calf muscle (origin) to the heel bone (insertion). There are two main types of Achilles Tendinopathy: mid-portion Achilles Tendonitis is in the middle of the Achilles Tendon, while Insertional Achilles Tendonitis is in the lower aspect of the tendon as it attaches to the heel bone (Calcaneus).
As the tendon attaches to the heel bone, it wraps around the curve of the calcaneus, attaching to the bottom of the heel. If there is pain or tenderness on the very bottom of the Achilles Tendon, it is referred to as an Achilles Enthesopathy.
The Achilles Tendon is the largest in the human body. Its function, along with the calf muscle, is to lift the heel off the floor and is used for most weight-bearing activities. It absorbs large amounts of force on impact activities such as hopping, running, and jumping. When running, the Achilles tendon absorbs up to 4-7 times your body weight, highlighting the tendon’s overall strength and capacity.
Approximately 6% of the general population reports Achilles tendon pain during their lifetime. Of these patients, roughly one-third will have insertional Achilles tendinopathy. Insertional Achilles Tendonitis may affect up to 9% of recreational runners. This article will cover the symptoms, treatment, and recovery of Insertional Achilles Tendonitis.
In acute episodes of Insertional Achilles Tendonitis, there is swelling and pain around the back of the heel bone. It is common to have these symptoms on one side only, but it is not entirely atypical to have pain in both heels.
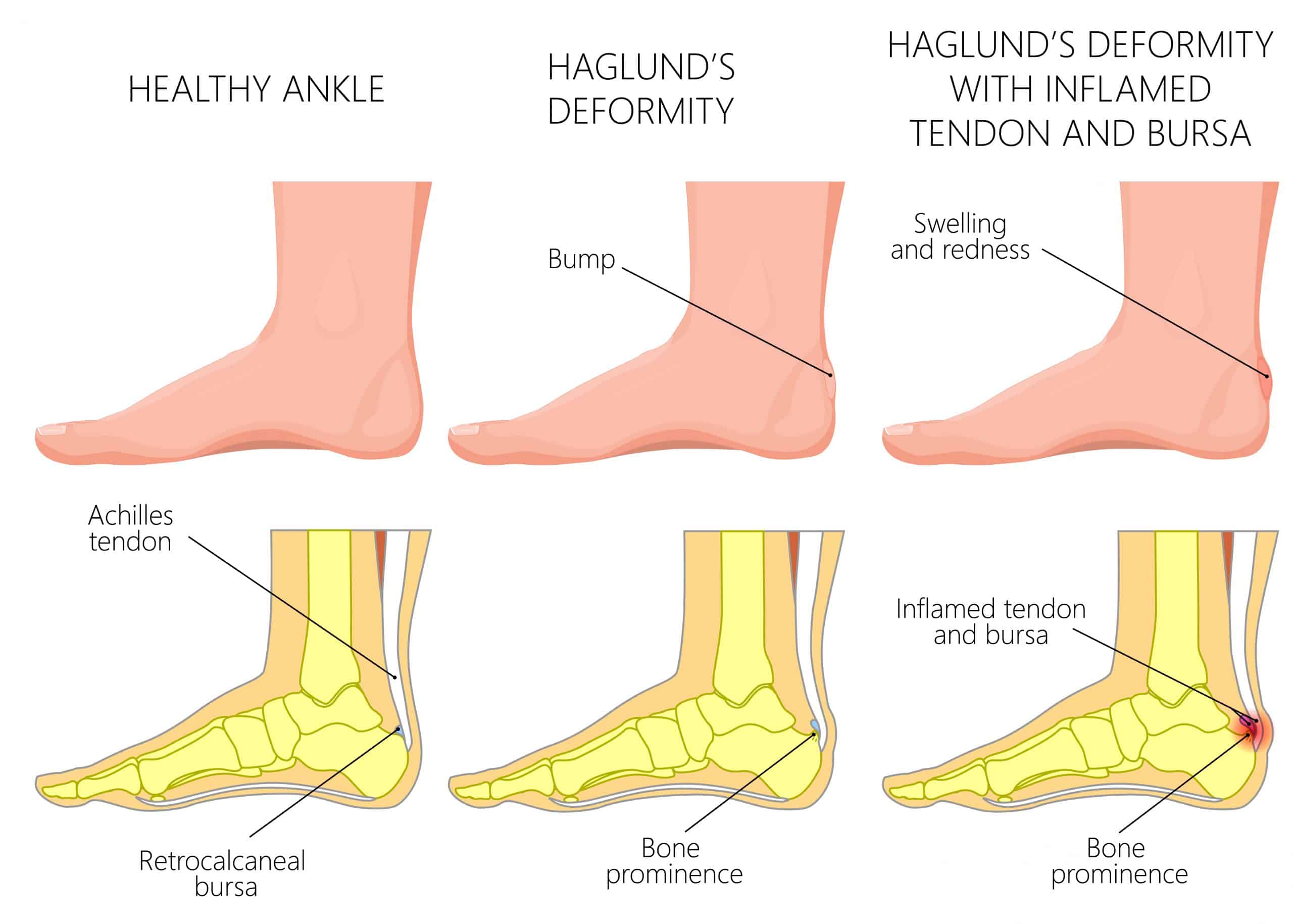
Pain may be constant with use and ease with rest, while sharper pain is common with hopping and running. It is common to have these symptoms alongside retrocalcaneal bursitis, and in these instances, there may be a visible bump of swelling at the back heel.
In sub-acute cases, we expect stiffness at the back and underside of the heel first thing in the morning that eases within 30-45 minutes after getting out of bed. It may be tender at the start of exercise, such as a run and improve as it warms up, while it may be sore again within an hour after the activity.
There can be pain when walking after sitting for a period of time, and low-profile shoes can exacerbate symptoms, while heeled shoes can provide relief. We do not expect pain all along the tendon as this is more indicative of Achilles Paratenonitis.
In chronic cases, it is common for there to be constant pain with all weight-bearing activities and worse on exertion.
This provides pain at the back of the ankle that can result from an extra bone, such as an Os-Trigonum or a bony growth on the heel bone called a Stiedas process. This is common in dancers and exacerbated by terminal Plantarflexion.
Related Article: Posterior Ankle Impingement Overview
A stress fracture of the heel bone can occur due to a repetitive overload of the heel bone. This is common in runners; an x-ray or MRI can be required for diagnosis. Common symptoms include heel pain with weight-bearing activities
Related Article: Over of Calcaneus Stress Fractures
A bursa is a sac of fluid at the back of the heel bone. Its primary function is to act as a cushion between the heel and the tendon. If it becomes irritated through overuse, it can become swollen and painful. It is not unusual to have Insertional Achilles Tendonitis and Retrocalcaneus bursitis simultaneously.
Related Article: Heel Bursitis
Insertional Achilles Tendonitis has a clear mechanical pattern and can be diagnosed by a healthcare clinician through a physical assessment. Clinical tests, such as the Achilles Tendon pinch test, are a reliable form of test. The pinch test involves squeezing the distal 2cm of the Achilles Tendon insertion to the heel bone; pain is indicative of a positive test.
At the same time, a Thompson Test may be carried out to rule out an Achilles Tendon Rupture, and a SLR test should be carried out to rule out Sural nerve irritation.
An ultrasound is a cost-effective imaging tool for diagnosing Insertional Achilles Tendonitis. At the same time, a more expensive method is an MRI which is the most accurate type of scan for Insertional Achilles Tendonitis.

Physical Therapy is the most effective form of treatment for Insertional Achilles Tendonitis. Depending on the stage of Insertional Achilles Tendonitis, treatment may differ but lets have a look at some of the treatments available.
Pain relief is important in the acute stages as it prevents secondary compensation injuries. This can come in the form of acupuncture, dry needling and massage.
Whether you have had an onset of pain from running or walking, altering the volume of these activities is important.
Strength training is the best form of rehabilitation, but if your pain levels are too high to do this, then it can be difficult to make progress.
Reducing your step count and keeping it consistent is helpful. Keeping your running pace and distance consistent can is also beneficial while maintaining 24-48 hours of rest between runs to allow the tendon time to recover.
Strength training is the best form of treatment for any form of tendonitis. The difference between Mid-portion Achilles Tendonitis and Insertional Achilles tendonitis rehabilitation is that for insertional tendonitis, all forms of calf raises are from the ground upwards.
Dropping below a step or neutral can lead to compression on the Achilles Tendon, leading to further irritation.
Heavy Slow Resistance training on a leg press or using weights at home can significantly improve function and pain relief.
Related Articles: Insertional Achilles Tendonitis Exercises
A simple heel raise placed inside your shoe can provide immediate pain relief.
The best inserts for Insertional Achilles Tendonitis are custom insoles that are formulated by foot specialists. They typically have a heel raise that shortens the Achilles Tendon alongside some medial arch support of the foot.
Steroid injections are generally avoided for this condition as moderate evidence suggests it can weaken the tendon over time. Adverse effects were reported in up to 82% of corticosteroid trials; these include tendon rupture. Any possible benefit of corticosteroid injection appears to be outweighed by potential risks.
A walking boot with heel raises inside is generally preferred to offload the tendon before recommencing Physical Therapy.
There is low-level evidence that Shockwave Therapy can be used as a primary treatment for Insertional Achilles Tendonitis, and we recommend using it alongside strengthening exercises.
In rare cases, surgery may be necessary for Insertional Achilles Tendonitis where it hasn’t responded after 3 months of appropriate Physical Therapy.
This can be in the form of debridement of the tendon, and a Haglund’s deformity may be shaved if present. Physical Therapy is conducted for 6-12 weeks to ensure an optimal surgery recovery.
Continuing to run with Insertional Achilles Tendonitis is possible, but caution is advised to prevent further injury or complications.
Insertional Achilles Tendonitis affects the lower aspect of the Achilles tendon as it attaches to the heel bone. This attachment point has less blood flow compared to the mid-portion and experiences compression against the heel bone, making continued running challenging.
Running with Insertional Achilles Tendonitis can cause increased pain levels; however, stopping running altogether may lead to deconditioning of the Achilles tendon, making it more difficult to return to running. The general principle is that it is acceptable to experience some pain in the Achilles tendon while running as long as this pain subsides within 24 hours of your run. If the pain persists beyond this timeframe, consider reducing your distance or pace during your next run.
To effectively manage Insertional Achilles Tendonitis while running, it is important to follow a carefully designed training plan that allows for progressive loading of the tendon while minimizing the risk of further injury. Here is an example of what a running programme with Insertional Achilles Tendonitis may look like:
Weeks 1-2: Pain management and initial rehabilitation with reduced running. During this phase, continue running but allow at least 48 hours between runs at a steady pace. Monitor pain levels the morning after a run, and consider reducing your running volume if you experience higher pain levels than normal. In this stage, the patient should begin isometric strengthening exercises for the calf muscles to help maintain and develop strength.
Weeks 3-4: Gradual return to running. Begin increasing the duration of your runs, starting with short distances at a slow pace and gradually increasing the duration by no more than 10% per week. Alternate between running and walking to reduce the stress on the tendon. In this stage, the patient should carry out isotonic calf and Achilles strengthening exercises to build strength and resilience in the tendon and surrounding muscles.
Weeks 5-8: Progressive loading and running. Increase running intensity by adding hill work or gradually increasing your pace while monitoring pain levels. Slowly add longer runs to your training schedule, adhering to the 10% rule for weekly volume increases.
Weeks 9-12: Return to regular training. Gradually return to your normal running routine, ensuring you maintain a balance between intensity, volume, and recovery. Incorporate cross-training activities, such as strength training, swimming, or cycling, to maintain your cardiovascular fitness.
It is essential to follow a comprehensive treatment plan, which may include physical therapy, strengthening and stretching exercises, and anti-inflammatory medications. Consult a medical professional, such as a Physical Therapist, to develop an appropriate plan tailored to your specific needs. They can guide you in managing your condition while running and help you make necessary modifications to your routine to minimize the risk of further injury.
In summary, while it is possible to continue running with Insertional Achilles Tendonitis, it is crucial to exercise caution and work closely with a healthcare professional to develop a personalized treatment plan to ensure a full recovery.
Are compression socks good for Insertional Achilles Tendonitis?
There is currently no evidence to suggest that compression socks are effective for treating Insertional Achilles Tendonitis. Compression socks are tight socks that you wear around your calf muscle to compress the calf and increase blood flow to the area. They are commonly used by long-distance runners to reduce calf pain when running and to help with recovery post-exercise. The theory is that compression reduces lactic formation. Still, there is limited evidence for this, and in fact, one paper highlights that compression socks may be a risk factor for developing Insertional Achilles Tendonitis
Should you stretch Insertional Achilles Tendonitis?
Stretching is not recommended for treating Insertional Achilles Tendonitis. The Achilles Tendon attaches the calf muscle group to the heel bone, and as it wraps around the back of the heel bone, there is a compression point between the tendon and the bone. When stretching the Achilles Tendon, it compresses the tendon against the heel bone, resulting in greater pain. Therefore, it is not recommended to stretch Insertional Achilles Tendonitis. We recommend strengthening exercises to alleviate your Insertional Achilles Tendonitis pain and using heel raises inside your shoes. If you have persistent Achilles Tendon pain, we recommend a consultation with a foot and ankle specialist.
This article is written by James McCormack, a Foot and Ankle Specialist who is an expert in treating Insertional Achilles Tendinopathy.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.