Boot For Sprained Ankle
Read More >
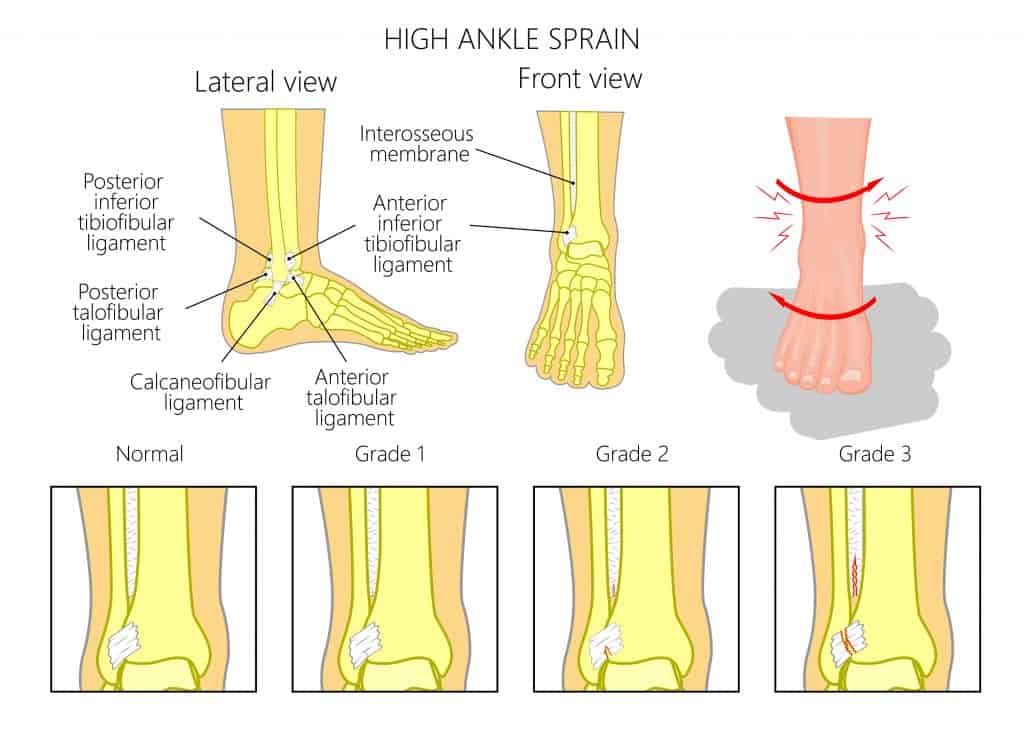
High ankle sprains (distal tibiofibular joint sprains) are ankle ligament injuries involving the ligaments connecting the tibia and fibula (shin bones), along with the syndesmosis. The ligaments attaching the tibia and fibula are called the Anterior Inferior Tibiofibular Ligament (AiTFL, the Posterior Inferior Tibiofibular ligament (PiTFL), the interosseous membrane, which is a large sheet of membrane that connects the tibia and fibula together along the shin, providing additional stability.
The AiTFL is a flat band that ranges from 12 to 20 mm at the front of the ankle. The PiTFL at the back of the ankle and the interosseous membrane is a large sheet that connects the tibia and fibula along the shin, providing additional stability.
In contrast, a low ankle sprain involves the ligaments inside or outside the ankle. The ligaments on the inner aspect of the ankle are known as the deltoid ligaments. In contrast, the ligaments on the outside of the ankle are the Anterior Talo-fibular Ligament (ATFL), Calcaneofibular ligament (CFL) and Posterior Talo-Fibular Ligament (PTFL).
High ankle sprains account for 1-18% of all ankle sprains, and these are often more complex than Low Ankle Sprains. As a result, they usually require a longer and more thorough rehabilitation. High ankle sprain recovery averages (2.5 vs 1.25 weeks) when compared to lateral ankle sprains in Division I collegiate football players.
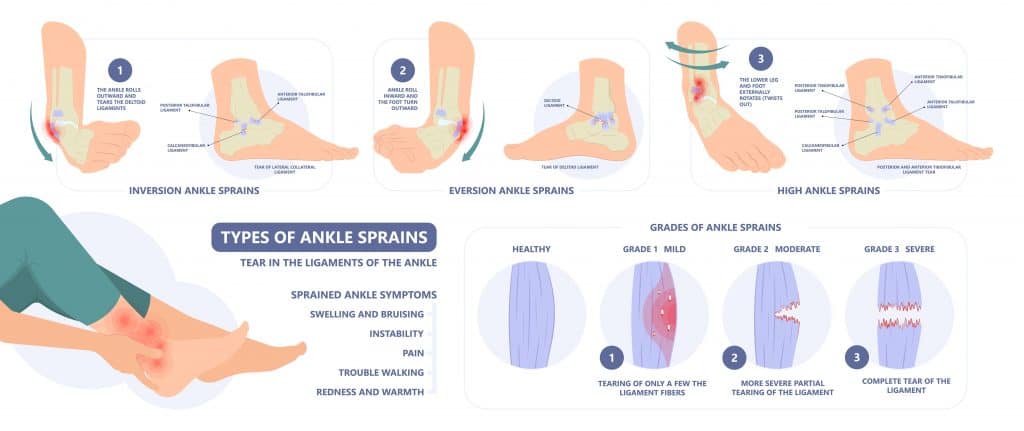
High ankle sprains can cause various symptoms depending on the size, location and type of sprain.
The most common symptoms of a high ankle sprain are pain at the front of the ankle and reduced range of motion, especially dorsiflexion. Activities such as walking, climbing stairs, running and hopping exacerbate the symptoms of a high ankle sprain.
In severe cases, there may be disruption to the syndesmosis leading to ankle instability, patients may be unable to weight-bear, and there may have been an audible crack or pop at the time of injury.
It is not unusual for minimal to no swelling but severe pain on hopping. The front of the ankle can be painful to touch, and in severe cases, this tenderness may be present on the lower 1/3 of the shin.
Forceful external rotation of the foot and ankle is the primary mechanism of injury for a high ankle sprain leading to separation of the tibia and fibula.
Common mechanisms of injury are:
High ankle sprains are more common in sporting activities 17-74%:
High ankle sprains are complex injuries that are often misdiagnosed in severity due to the complex nature of the injury. As a result, it is important to see an experienced physical therapist for a clinical examination in ankle injuries. This form of examination is often sufficient for a clinical diagnosis of mild or Grade 1 high ankle sprains. Still, a clinical examination and imaging tests are typically required in higher-grade sprains.
A clinical examination should contain two special tests are often used; the Squeeze test and external rotation test.
The Squeeze test, where the proximal end of the tibia and fibula are squeezed together with pain provocation, indicates a positive test. The squeeze test has a sensitivity of 30% and a specificity of 93.5% for a high ankle sprain.
The external rotation test requires the therapist to take the ankle into a neutral posting and externally rotate the foot. If there is a pain in the anterolateral ankle, it is a positive result with a sensitivity of 20% and a specificity of 84.8% for a high ankle sprain.
An MRI is the gold standard scan for high ankle sprains. It will provide information on any soft tissue damage such as a ligament tear or compromise to the syndesmosis.
In addition to this, it can detect any bony injuries such as a fracture to the tibia and/or fibula
An ultrasound is a cost-efficient alternative to an MRI and will provide live feedback on the status of the AiTFL & PiTFl. Although it can detect bony injuries, it is not as sensitive as an MRI scan.
An x-ray is unable to detect the integrity of ligaments but it can be useful for ruling out other conditions.
In the early stages after a high ankle sprain (0-3 days), protecting the joint as much as possible is important. Home remedies during this period include compression taping, keeping the ankle elevated and applying ice to help with pain relief. In severe cases that involve compromise to the syndesmosis, it is recommended to immediately use a walker boot with crutches to protect the ankle joint.
Treatment with a Physical Therapist should begin as soon as possible. Physical therapy may involve soft tissue massage to restore the range of motion, and rigid ankle taping may be applied to support the ankle, which can help normalise walking gait.
A rigid ankle brace may be used instead of rigid taping if required, allowing the patient to mobilise while protecting the site of injury, which helps reduce swelling and maintain good blood flow.
Progressive strengthening exercises alongside balance and proprioception exercises are part of a standard rehabilitation program. A Physical Therapist specialises in knowing when and how to progress these exercises throughout the recovery process.
When entering the later stages of rehabilitation, change of direction exercises, hopping protocols, and sport-specific exercises are added.
Overall, there is currently no high-level evidence on the most effective management for a high ankle sprain and most approaches are based on slow progressive strengthening and stability exercises.
Surgery may be required in severe cases where the high ankle ligaments are completely ruptured or clinically insufficient. This typically involves a surgical fixation using a screw and/or wire to provide stability to the joint. A rehabilitation program follows this.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating High Ankle Sprains.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.