Shin Splints Massage
Read More >
Shin Splints or Medial Tibial Stress Syndrome affects the inner (medial) aspect of the tibial bone, generally in the lower 1/3 and surrounding muscles. There are slight anatomical differences in each person, but primarily the Soleus muscle, Posterior Tibialis muscle and the Flexor Hallucius Longus muscle attach to the medial aspect of the tibia.
It is believed that if stress is applied to the area where these muscles attach to the bone (periosteum), it causes inflammation and irritation, leading to Shin Splints. This is a progressive condition; the bone can become compromised if it deteriorates, leading to a stress fracture.
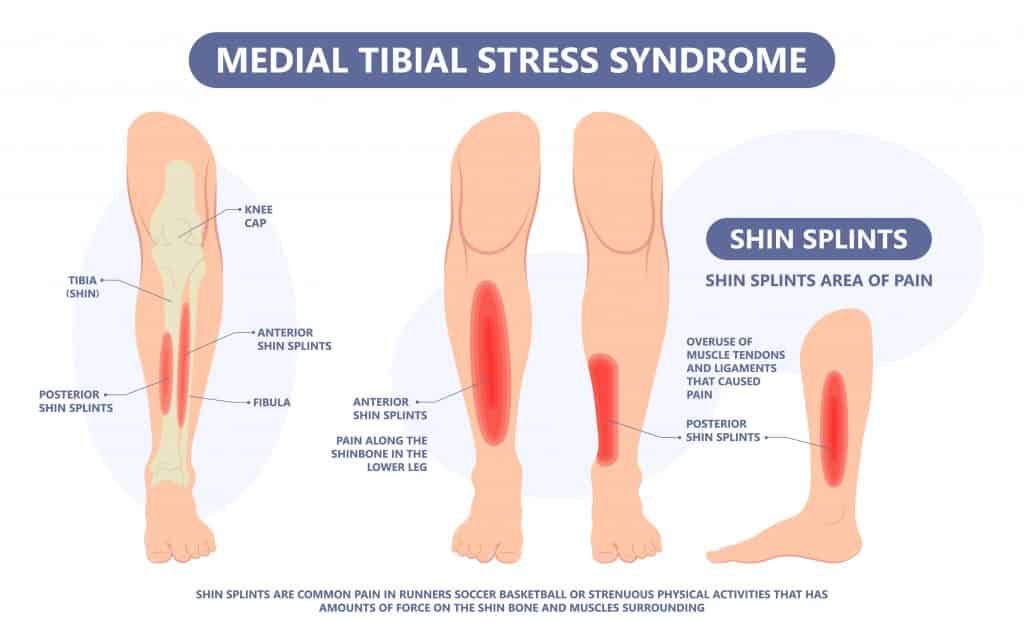
Shin Splint pain is felt along the inner aspect of the shinbone. If you run your hand along the bone, there may be visible bumps, lumps or swelling.
It is painful when walking or running, mainly uphill or on hard surfaces. In mild cases, it is not unusual for the pain to ease and go away during a run before returning when you stop. As the condition deteriorates, it becomes constantly painful with impact activities.
Symptoms can appear on both sides and should improve with rest. Activities such as Basketball, Jump Rope Skipping and Running will likely worsen symptoms. There may be some night pain if you have aggravated the shin bone during the day.

A sudden change in activity levels is the most common cause of Shin Splints.
This can vary from walking to running, but increased volume, speed or intensity of impact activity are primary causes.
If there is no change in activity levels, then a biomechanical cause, such as flat feet or poor foot control, can alter where the force is applied to the shinbone. It can lead to more pressure on the medial aspect of the Shin.
There is no evidence to suggest that having tight calves is a risk factor for Shin Splints, but it can be rationalised clinically.
Other causes to consider are poor footwear selection; this can be inadequate support or that they have become too worn.
Poor hip control can overload the shin, and females are more likely than males to get medial tibial stress syndrome, according to Newman et al., 2013.
A clinical assessment by a Physical Therapist or a Sports Doctor is the Gold Standard form of diagnosis for Shin Splints. A clinical interview is followed by a physical assessment of a patient’s foot control, strength and mobility.
The tibia is palpated for pain along the medial line, and a hop test is performed. A tapping test may be carried out to rule in or out a potential stress fracture.
An x-ray cannot diagnose Shin Splints; if imaging is required, this is an MRI Scan. There may be evidence of periosteum or bone marrow oedema on an MRI, but the specificity varies between 33-100%.

Shin Splint’s treatment should be multifaceted as one intervention is unlikely to resolve the symptoms. Treatment should be under the guidance of a Physical Therapist.
In the initial phase, identifying the causes of pain is essential so that they can be limited or altered to help control your pain levels. Following assessment stretches, strengthening and stability exercises are often recommended. Massage and foam rolling can be performed to the surrounding muscles for pain relief.
Taping may be applied to help reduce the pain levels; this can be done with rigid zinc oxide or KT Tape. Other forms of pain relief that can be recommended are ice sleeves or compression socks.

Running gait analysis is beneficial for identifying factors contributing to the cause of your shin splints, such as poor hip control and rapid pronation moments of the foot. These can be addressed with running re-training strategies, insoles, stability trainers and strengthening exercises.
In very irritable cases, a walker boot may be required for 2 weeks before recommencing rehabilitation. Surgery is rarely recommended due to poor outcomes, but periosteal stripping or a fasciotomy is the most common.
Shin Splints are worse at night because of a build-up of irritation during the day. When you rest at night this becomes more noticeable, with some patients describing a throbbing sensation, even at rest.
If you sleep on your side, you should try placing a pillow between your knees and shins so there is no direct pressure on your shin bones. If you sleep on your back, place a pillow under your knees; if you sleep on your front, place a pillow under your ankles.
In our experience, Flat Feet is a risk factor for Shin Splints. Biomechanically, flat feet increase weight distribution through the inner aspect of the foot, shin and knee, increasing force on the medial aspect of the shin bone and resulting in a greater risk of Shin Splints. Evidence suggests that flat feet can accelerate cartilage change in the ankle and knee due to high pronation forces through the foot when walking or running.
A study by Bennett et al., 2001 looked at the foot profile of 125 high-school cross-country runners and found that those who developed Shin Splints significantly reduced medial arch height. This study indicates that having Flat Feet can cause shin Splints.
When we walk or run, in an ideal world, there is an even distribution of force across our feet and legs. As our foot moves through the gait cycle, force moves from the foot’s outer aspect to the foot’s inner aspect until we push off, with most of our weight going through our big toe. When someone has a flat foot, this force is not as evenly distributed, and most force is placed on the inner aspect of the foot, leading to greater force being applied to the inner aspect of the shinbone.
The impact of walking and running combined with uneven force distribution through the inner aspect of the shin causes Shin Splints. Depending on the cause of your Flat Foot, we can strengthen the foot to redistribute forces or use a stability trainer or insoles to assist a Flat Foot passively.
In our experience, the best way to prevent Shin Splints with Flat Feet is to carry out regular strengthening exercises of your feet and ankles, wear cushioned supportive footwear and mix your training between impact and non-impact activity.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Shin Splints.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.