Knee Pain Location Chart
Read More >
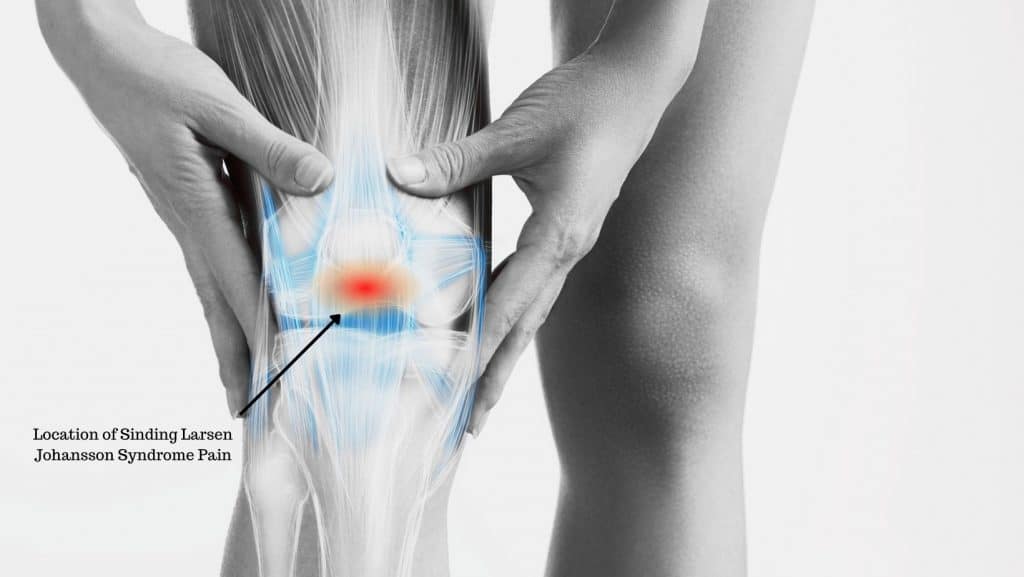
Sinding Larsen Johansson Syndrome (SLJ) is an injury causing pain and swelling in the bottom tip of the kneecap. It affects children and teenagers who are active in sports and is most common between the ages of 10 and 14.
SLJ affects the growth plate at the bottom tip of the kneecap where the patellar tendon attaches. It occurs when repetitive tension is placed on the growth plate. This can be from repetitive traction from the patellar tendon during running, jumping and impact activities.

A healthcare professional such as a family doctor or physical therapist will ask about the symptoms and history of the injury.
A physical examination will assess where the pain is. And if symptoms can be reproduced with the aggravating movements: stretching the quadriceps, squatting or jumping.
A clinician may refer the patient for imaging to confirm the diagnosis.

It is often misdiagnosed as Patellar Tendonitis, which occurs at the same location but is more common in older teens and adults, and Osgood Schlaters, where pain is lower down at the patellar tendon insertion to the tibial tuberosity.
While radiology is not always necessary there are three forms of imaging that can provide confirmation of suspected Sinding Larsen Johansson syndrome:

X-ray is the least sensitive form of imaging for SLJ. It is able to rule out a fracture, or stress fracture, of the patella or shin bone, which might give similar symptoms.
An MRI of a suspected SLJ will show inflammation which can indicate the injury to the growth plate.
Ultrasound is the most informative, cost-effective and safest imaging technique to confirm SLJ.
It is a less stressful assessment for a child, there is no radiation, and the parent can be with them throughout. The scan can be done dynamically with an explanation as the knee is moved.
To manage SLJ symptoms, we recommend reducing impact activities, increasing rest between activities and trying alternative non-impact sports such as swimming or rowing. Generally, with activity modification, symptoms in mild cases can improve considerably in 6-8 weeks.
Patients can ice their knee for for pain relief for 10-15 minutes, 3-4 times daily especially after sport. And take non-steroidal anti-inflammatories, if the child is over 12 years old and it is safe to do so.
Stretches, foam rolling and massage can all be used for effective treatment of SLJ. These treatments relax the quadriceps muscles reducing the tension on the growth plate.
Additional exercises may be prescribed to strengthen other muscles to offload the quadriceps muscle. Typically this will be working on the posterior chain of muscles: glutes, hamstrings, and calf muscles. It is a good opportunity to address imbalances of strength and flexibility or any poor movement control.


Taping the knee can be effective for pain relief. Applying either elasticated tape, such as Kinesio Tape, or ridged tape can help to make the knee feel more supported.
This is useful when the condition is less severe and activity can be continued at a modified volume and/or intensity.
Click to see How to Apply Kinesio Tape for Sinding-Larsen Johansson syndrome.
There are two kinds of knee braces that can be used. An elasticated knee brace (shown) will offer compression and might make the knee feel supported, or an infrapatellar knee strap.
When activities are reduced but not completely restricted, straps and braces are often used to make the activity less painful.


SLJ can persist until the growth plates close, usually in the late teens. However, with the appropriate management, symptoms can be alleviated while the child is still growing.
Symptoms can be reduced with activity modification and correct management within 6-8 weeks.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Knee Pain.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.