Shin Splints Cycling
Read More >
Posterior Shin Splints, which is also known as Medial Tibial Stress Syndrome, is a condition that affects the inner aspect of the shin bone, and it accounts for up to 35% of running injuries.
One of the primary causes of Posterior Shin Splints is repetitive overload, where excess force due to certain running styles is placed on the shin bone leading to inflammation and pain.
A long thin muscle runs along the inside of the shin bone calf, the Tibialis Posterior muscle, which attaches to the medial arch of the foot. If this weakens over time, it can make the foot flatter and change the direction of the force applied to the shin bone when walking or running.
Continuous overload of the inside of the shin bone causes irritation and inflammation of the medial shin bone, called Posterior Shin Splints.
Without the correct treatment, Posterior Shin Splints can persist for a long period of time and hinder your return to impact sports. Throughout this article, we will explain the symptoms, causes and treatment of Posterior Shin Splints to get you back to doing the things you love.

The symptoms of Posterior Shin Splints are characterised by exercise-induced pain along the posteromedial border of the lower 2/3 of the tibia.
Patients report a sharp pain on impact when running or jumping along the inner aspect of the shin, while there may be a dull ache when walking. Pain normally eases at rest but in severe or persistent cases, there may be a low-level pain at rest.
There is rarely any visible bruising to the shin bone, while there may be some mild swelling in severe cases. Walking or running uphill can aggravate the symptoms of Posterior Shin Splints.
Pain on single leg hopping and/or swelling may indicate a tibial stress fracture.

Weakness to the posterior tibial tendon is one of the primary causes of Posterior Shin Splints as it results in flattening of the foot and more significant stress being applied to the inner shin.
A flat foot can increase the risk of developing Posterior Shin Splints due to increased force being applied to the inner aspect of the tibia.
Overuse or a sudden increase in impact activity can also cause Posterior Shin Splints.
Other causes of Posterior Shin Splints include poor footwear, high BMI and biomechanical faults in someone’s gait.
Finally, weakness in the surround muscles of the leg and hip can overload the shin causing pain and discomfort.
A Podiatrist or a Physical Therapist can diagnose Posterior Shin Splints in a clinic following a subjective and physical examination.
Based on a patient’s symptoms of shin pain during or within 24 hours after impact activity and tenderness along the medial aspect of the bone of at least 5cm. If the clinician is unsure of the diagnosis, they might refer a patient for imaging.
A standard x-ray can rule out any bone stress response, such as a stress fracture, while an MRI can provide information on the bone and the health of the surrounding soft tissues.

Home treatment for Posterior Shin Splints should include reduced time on your feet, including walking and running. If you have mild pain, you can continue to run but take at least 48 hours of rest from impact activity to allow the bone to recover. Icing your shin pain is an excellent analgesic, while non-steroidal anti-inflammatories such as Ibuprofen reduce inflammation in the shin.
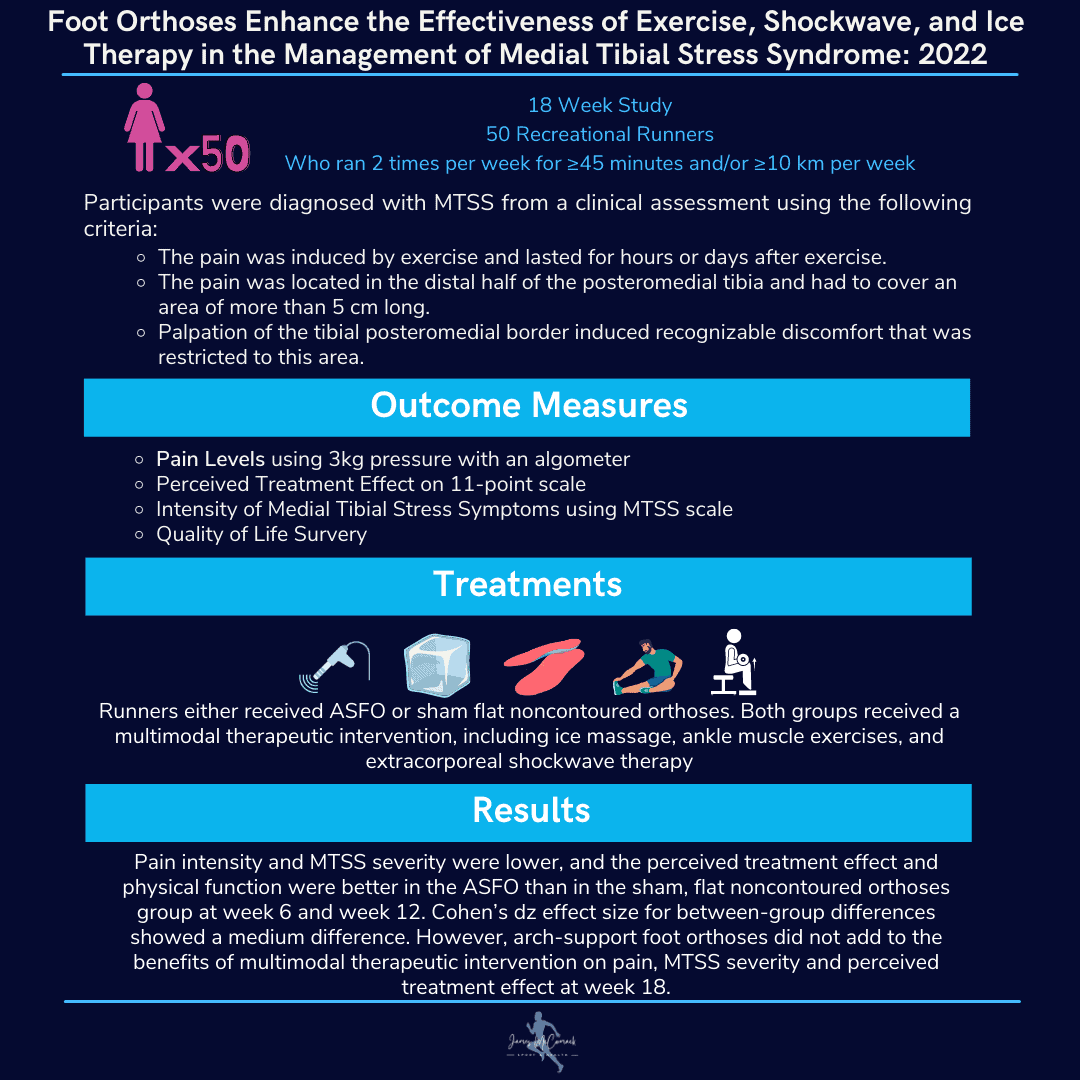
Physical Therapy can identify muscular imbalances that may be causing an overload of the medial shin. In contrast, a gait analysis can identify the level of support required from footwear or the necessity for custom insoles.
A thorough rehabilitation protocol should include stretching the calf muscles and strengthening the ankle stabilisers as well as the hamstring and gluteal muscles.
In severe cases, a period in a walker boot of 2-4 weeks may be recommended to reduce inflammation and irritation of the bone before recommencing Physical Therapy.
Consider non-impact activity such as cycling as a replacement for cardiovascular exercise.
Physiotherapy with James McCormack
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Posterior Shin Splints.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.