Morton’s Neuroma Exercises
Read More >
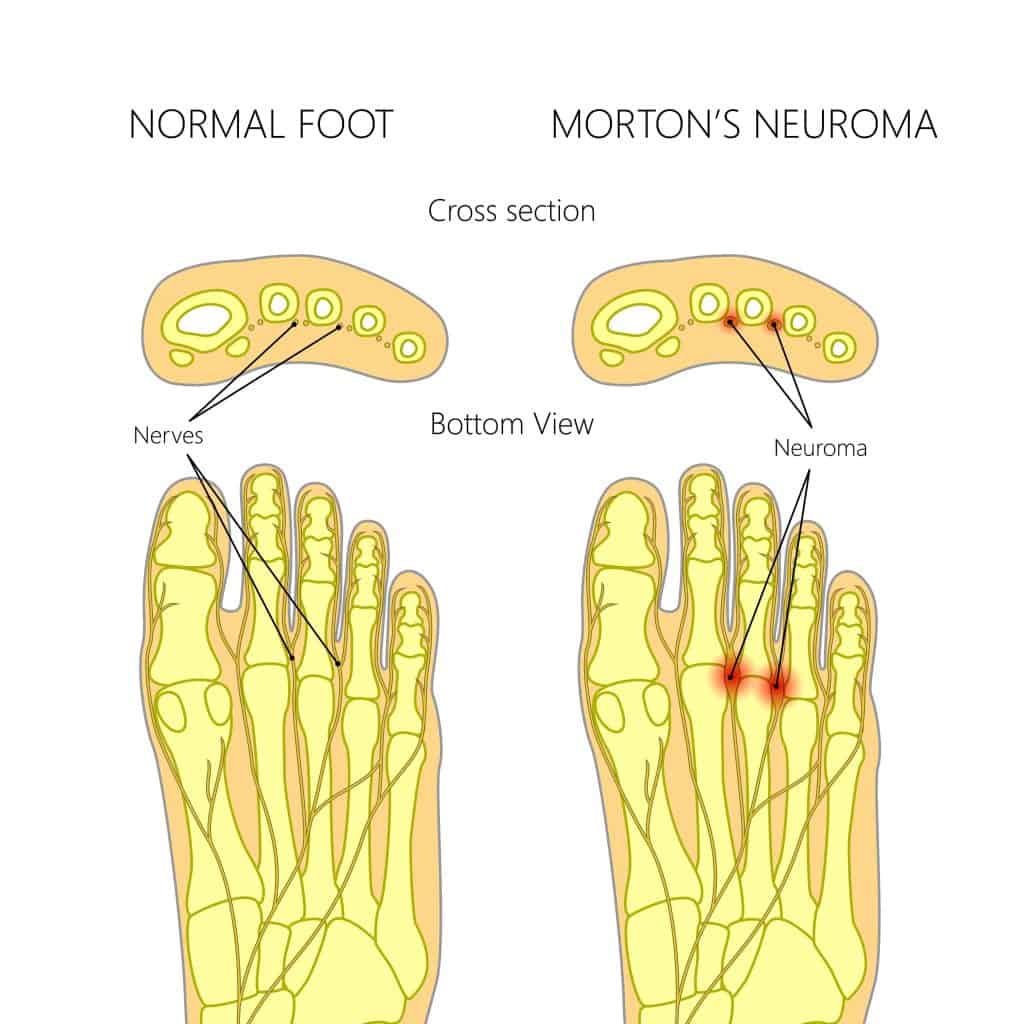
The common digital nerves that come from the lateral and medial plantar nerves pass through the web spaces of the toes of the feet. They provide nerve supply to the toes, and if they are damaged or injured, they can cause pain and numbness in the web spaces and toes. This commonly occurs between the 3rd and 4th toes and is called Morton’s Neuroma.
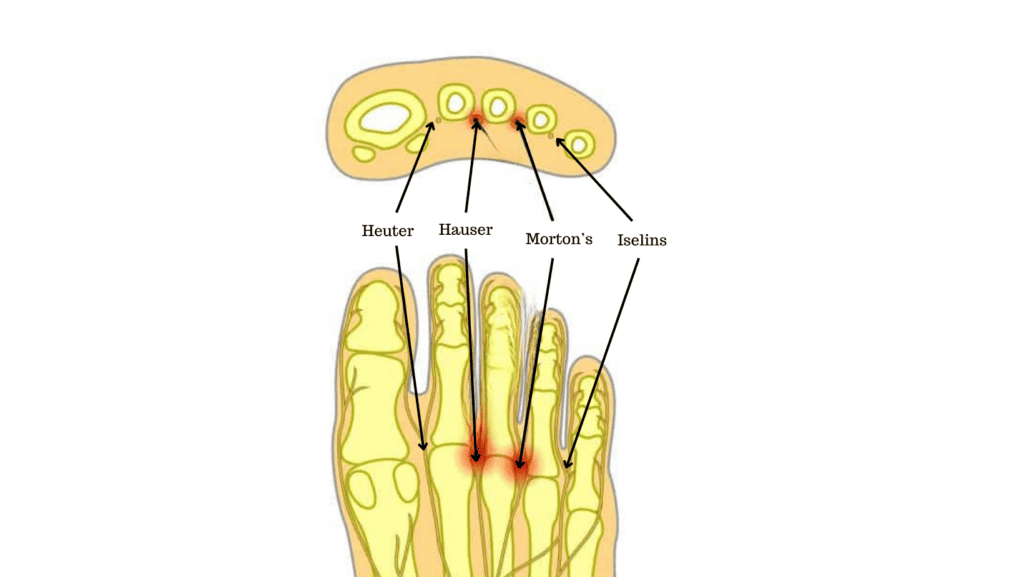
It is commonly mistaken that inflammation and pain in web spaces are known as Morton’s neuroma, but this is incorrect. The more appropriate terms for the digital nerves are Heuter (Between 1st and 2nd), Hauser (between 2nd and 3rd), Morton’s (between 3rd and 4th) and Iselin (between 4th and 5th).
A Morton’s neuroma is a painful condition affecting the ball of the foot. Interdigital nerves between the toes become painful and swollen, leading to numbness and pain in the forefoot.
People with neuromas often describe the pain sensation as similar to having a pebble in their shoe. Symptoms can often be a burning sensation with some tingling and pins and needles, while it is uncommon to experience bruising.
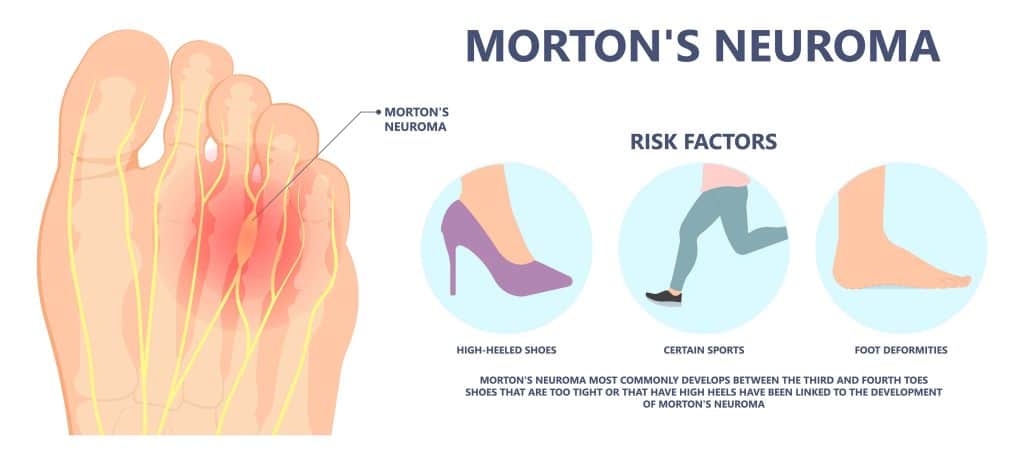
Morton’s Neuroma symptoms are aggravated by wearing high heels, tight shoes, or repetitive impact to the forefoot through activities such as running and impact sports.

There are several potential causes of Morton’s Neuroma:
Footwear: Wearing ill-fitting shoes that are too tight in the toe box can compress the web space and pinch the neuroma, leading to pain and swelling.
High Heels: Wearing high heels can lead to excess weight-bearing and pressure on the forefoot
Bunions: A mechanical or genetic bunion can lead to excess pressure on the 2nd-5th metatarsals. This often leads to a drop in the metatarsal heads and compression of the interdigital nerves.
Impact Sports: Repetitive impact of the forefoot from jumping or high-impact sports can lead to a Morton’s Neuroma
Flat Feet or High Arches: biomechanical changes in foot movements as a result of flat feet or high arches can lead to a Morton’s Neuroma
No hereditary or genetic links can directly lead to Morton’s Neuroma.
Clinical Assessment: An assessment by a medical professional such as a Physical Therapist or a Podiatrist is 98% sensitive compared to using an ultrasound scan to detect Morton’s Neuroma. The most accurate clinical test for Morton’s Neuroma is the Thumb Index Finger Squeeze test which has 96% accuracy and sensitivity compared to the Mulder’s Squeeze test, which has 61% sensitivity and 62% accuracy.
X-ray: An X-ray is useful to rule out any other potential causes of forefoot pain, but it cannot be used to diagnose Morton’s Neuroma.
Ultrasound and MRI: A systematic review in 2015 by Bignotti et al, concluded that an ultrasound scan is of equal accuracy to an MRI in the diagnosis of Morton’s Neuroma. It also benefits from being more cost-effective than an MRI.
1: Reduce time on your feet where possible
2: Ice massage to reduce pain levels
3: Wear comfortable, cushioned, wide-fitting shoes
4: Take anti-inflammatories
5: Try an off-the-shelf insole with a metatarsal dome
6: Maintain a healthy weight
7: Non-impact exercise
There is currently no evidence to support using apple cider vinegar to treat Morton’s Neuroma despite popular recommendations on social platforms.
There is no singular best form of treatment for Morton’s Neuroma. The first stage is to get the correct clinical diagnosis and then seek treatment from a medical professional. We will discuss all treatment options in this article and their benefits.
Massage: This can provide pain relief for Morton’s Neuroma as it relaxes and stretches the soft tissues surrounding the forefoot.
Physical Therapy: This is likely to incorporate rehabilitation exercises to correct foot and ankle stability and to optimise the foot biomechanics.
Orthotics: A foot specialist can create custom orthotics to offload the forefoot and metatarsals, reducing the pressure on the interdigital nerves. A forefoot pad or dome may be placed on the orthotic to gap the space between the toes, reducing the inflammation levels of the neuroma.
Cryosurgery involves the insertion of a probe into the neuroma and effectively freezing the neuroma. In a study by Caporusso et al, of 20 patients who had cryosurgery for Morton’s Neuroma, 38.7% were completely pain-free after treatment, and 42.5% had reduced pain levels.
Ultrasound-guided radiofrequency Ablation involves the insertion of a probe into the interdigital neuroma and generating high-frequency currents into the neuroma leading to heat necrosis. Ultrasound-guided radiofrequency ablation is 85% effective, according to a study by Chutter et al.
Cortisone Injections are effective in reducing pain levels for Morton’s Neuroma. Cortisone injections are recommended for cases not improving from Physical therapy and orthotics. Injections help by providing steroidal anti-inflammatories directly into the interdigital nerve, reducing swelling and pain levels. They are performed under ultrasound guidance.
Surgery can be performed to remove the neuroma or a surgical decompression may be performed to remove surrounding structures that may be compressing the interdigital nerve.
If Morton’s Neuroma is left untreated, it is highly unlikely to go away. It is recommended that you see a medical professional to get the correct diagnosis, as there are several conditions that present with similar symptoms. Once the correct diagnosis has been achieved, symptoms might improve with some of the home remedies we have suggested or treatment guided by a medical professional may be necessary.
If you have a medically diagnosed Morton’s Neuroma and it is getting worse, then it is recommended to see a Podiatrist or foot specialist Physiotherapist for guided treatment. If this fails, orthotics may be required or a cortisone injection. If Morton’s Neuroma continues to get worse, then surgery may be required.
It takes 4-6 weeks for a Morton’s Neuroma to heal when treated appropriately by a medical professional. Recovery from Morton’s Neuroma may not occur as symptoms can deteriorate without the correct medical care.
A Morton’s Neuroma is located in the forefoot and is characterised by pain, numbness, and tingling in the forefoot and toes. Plantar fasciitis is characterised by pain on the heel bone and/or along the arch of the foot. Morton’s Neuroma does not directly provide pain on the heel bone, although it may be possible that someone with a Morton’s Neuroma alters their gait to put more weight through their heel to avoid putting pressure on their painful forefoot. This compensation pattern can lead to the development of Plantar fasciitis.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Morton’s Neuroma.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.