Extensor Tendonitis: Foot
Read More >
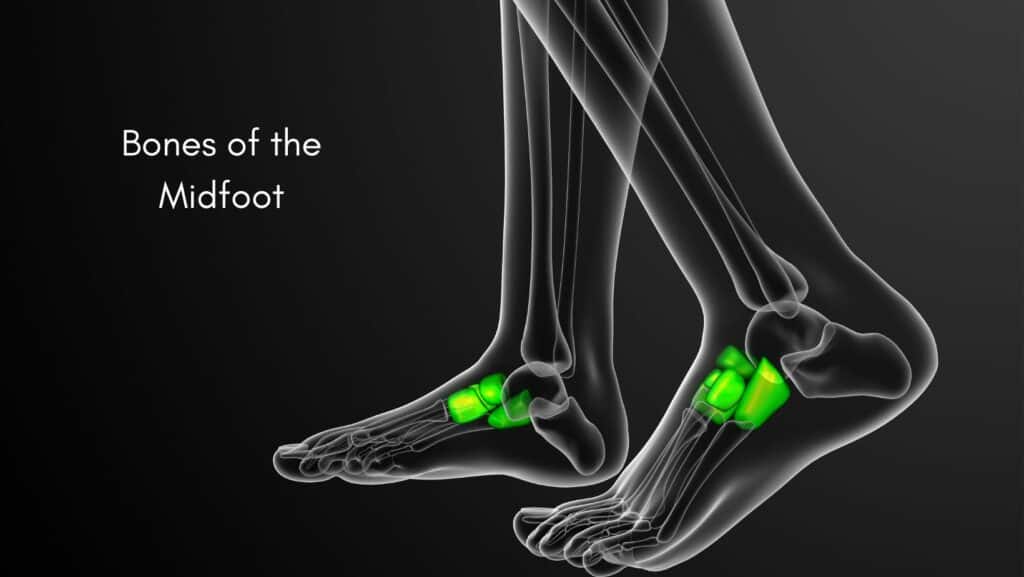
The Midfoot is the part of the foot connecting the hindfoot to the front of your foot, consisting of several bones and joints. Each bone within the Midfoot is surrounded by hard cartilage whose function is to protect the bone. Due to the location of the Midfoot, it takes a lot of strain when weight bearing, walking and running, so there are naturally some changes within the area as we age. If the cartilage in the Midfoot wears down, it can become painful and inflamed, leading to Midfoot Arthritis.
The symptoms of Midfoot Arthritis include pain in the Midfoot which is worse in the morning and with activity. There is often stiffness in the Midfoot first thing in the morning or when walking after sitting for periods.
There may be swelling on the Midfoot, while symptoms are aggravated by standing and impact activities such as walking and running.
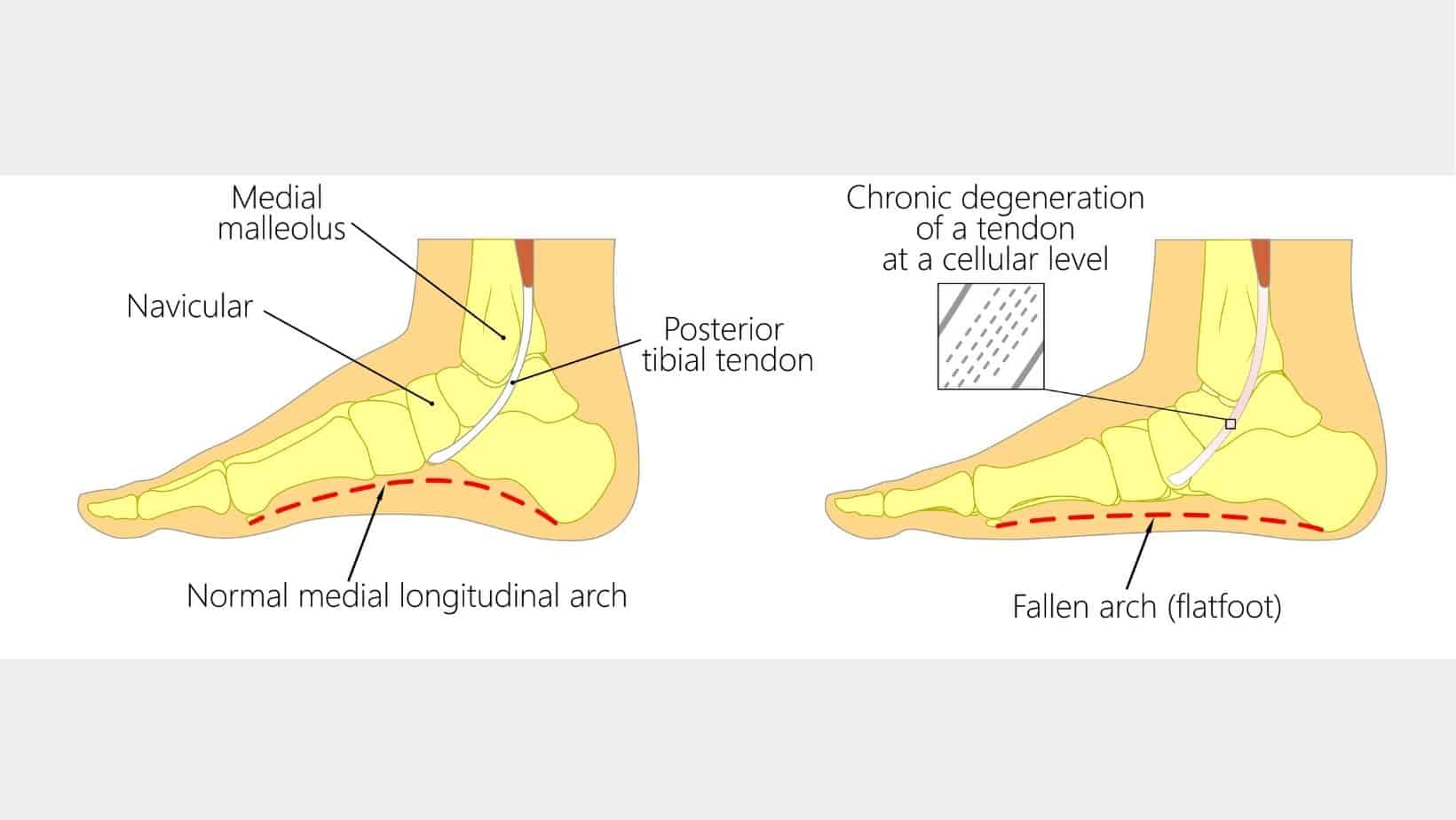
Midfoot arthritis can result from foot deformities such as a flat foot as this alters where force is applied in the foot, in this instance, the Midfoot. Trauma to the foot, such as Midfoot sprains and a fall, can accelerate the speed of onset of Midfoot arthritis.
Weakening of muscles, such as the Posterior Tibial Tendon, can lower the arch height of the foot and cause Midfoot arthritis. In some cases, Midfoot arthritis can develop with no specific mechanism.
Other causes of Midfoot arthritis include obesity and Rheumatoid Arthritis.
Midfoot arthritis can be diagnosed in a clinic by a Sports Doctor or a Physical therapist following a Physical Examination. If the clinician is uncertain of the diagnosis or would like to rule out other potential causes of midfoot pain, they may refer you for an x-ray.
An x-ray can identify cartilage loss and joint space indicative of midfoot arthritis. At the same time, an MRI may be requested to rule out other soft tissue injuries contributing to your pain.

Exercise rehabilitation under a Physical Therapist’s guidance is a highly effective treatment for Midfoot arthritis. Treatment includes strengthening exercises of the foot and ankle, balance exercises and a mobility programme.
Non-impact exercise such as swimming and cycling is highly effective for improving cardiovascular fitness and managing weight, as obesity plays a significant role in pain levels for this condition.
Supportive stability trainers provide comfort to the foot, while a gait analysis can identify insoles’ need to support the foot.
In some cases, an injection such as a corticosteroid injection may be required to reduce pain levels. Some doctors prefer hyaluronic acid, but this should be discussed on a case-by-case basis.
This is not medical advice and we recommend a consultation with a medical professional such as James McCormack before trying any of these exercises. James offers Online Physiotherapy Appointments for £45.
Related Article: Posterior Tibial Tendonitis – Conditions that cause pain on the top of the foot