Read More >
- Anterior Ankle Impingement - July 24, 2022
- Tarsal Coalition - October 12, 2022
- Sural Nerve Pain - October 3, 2022
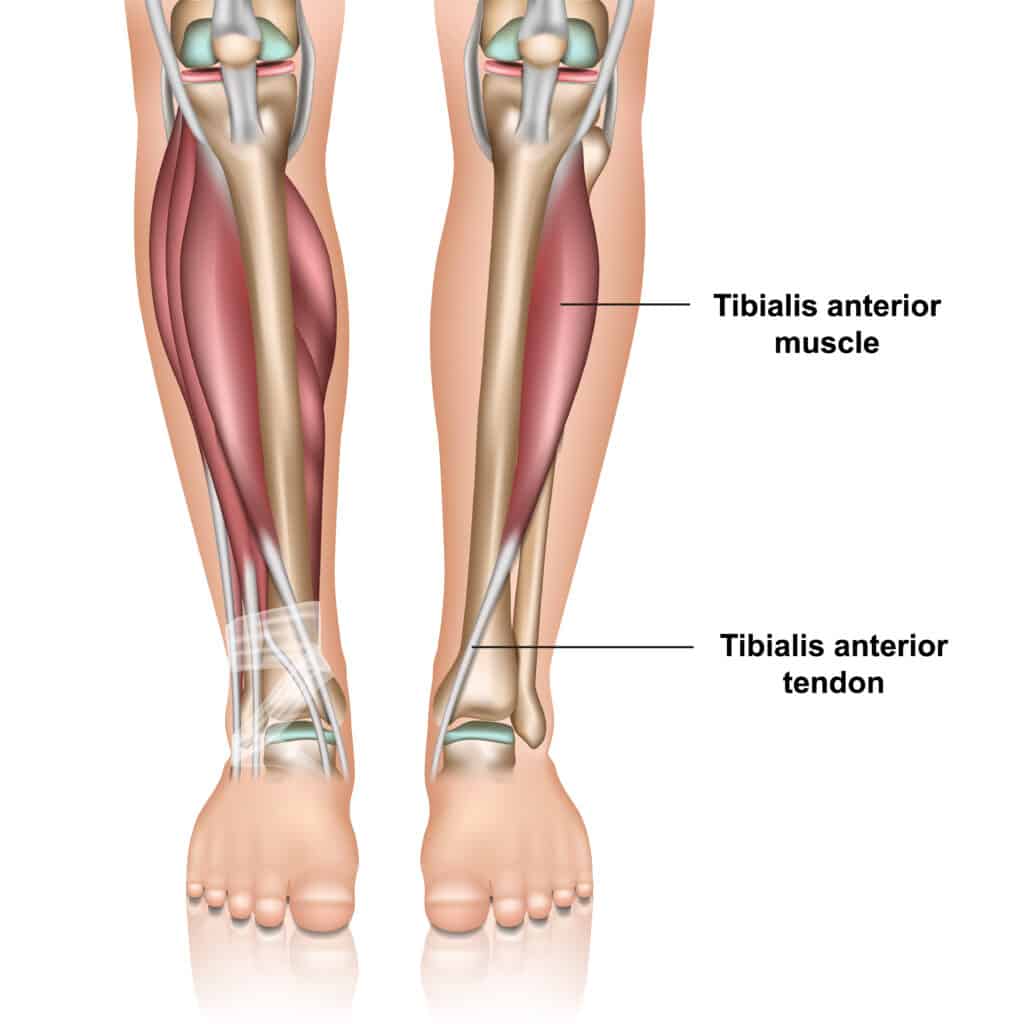
Located on the front of the tibia, the Tibialis Anterior muscles play a crucial role in the gait cycle and foot and ankle stability. This article will explore the anatomy and function of the Tibialis Anterior and the potential causes and treatments for Tibialis Anterior Tendonitis.
Tibialis Anterior: Anatomy
The Tibialis anterior muscles’ origin is on the anterior distal one-third, moving down the front of the tibia and across the ankle to attach onto the medial cuneiform and the base of the first metatarsal. Interestingly, the Tibialis Anterior tendon is the most medial tendon of the foot and ankle.
The Tibialis anterior is innervated by the deep peroneal nerve (deep fibular nerve), which arises from the common peroneal (fibular) nerve.
The Tibialis anterior can have physiological variants, with the tendon splitting into two in some cases and attaching to the medial cuneiform and 1st metatarsal separately.
Function
Dorsiflexion is the upward movement of the foot, and the Tibialis Anterior is the strongest dorsiflexor. As a result, the Tibialis Anterior play a vital role in the gait cycle by lifting the foot to clear the ground during the swing phase of gait.
The Tibialis Anterior plays a role in the inversion (turning inwards) of the foot alongside the Posterior Tibial Tendon while also helping to stabilise the medial longitudinal arch of the foot through the gait cycle.

Causes of Tibialis Anterior Tendonitis
As the Tibialis anterior is the primary dorsiflexor of the foot, a sudden change in activity levels, such as increased volume of walking, running, or impact exercises, can overload the tendon and lead to Tibialis anterior Tendonitis.
Wearing high heels or switching to a shoe with a high heel drop can require more dorsiflexion in the gait cycle, leading to an overload of the Tibialis anterior.
Running or walking uphill can place extra demand on the Tibialis anterior, resulting in Tibialis anterior tendonitis.
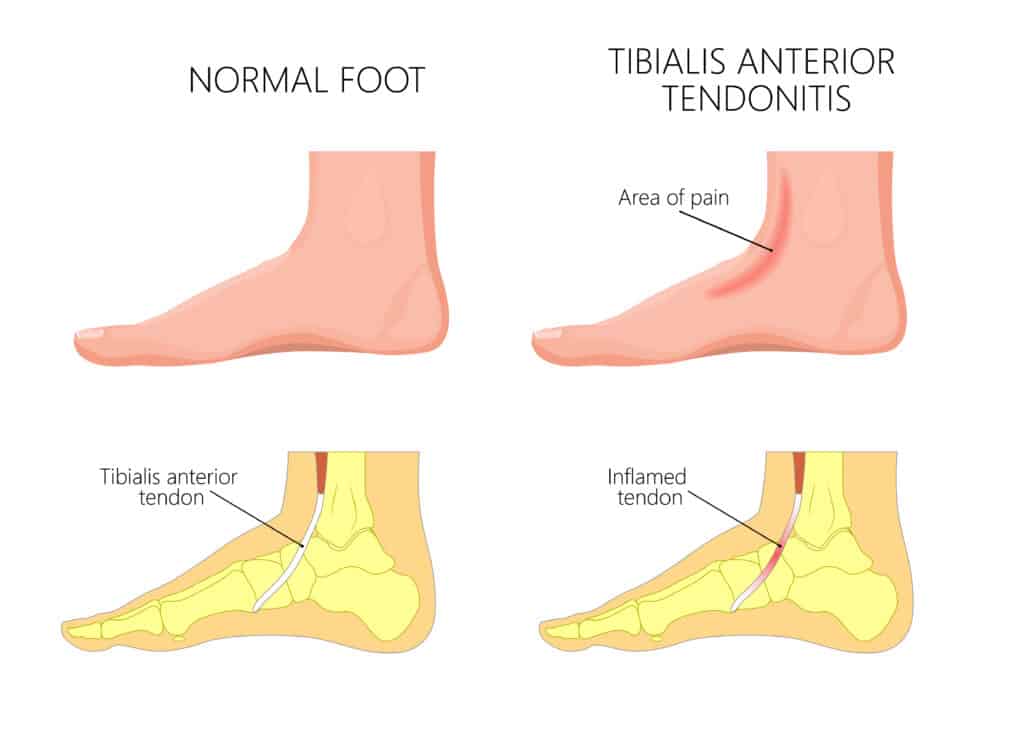
Tibialis Anterior Tendonitis: Symptoms
Tibialis Anterior Tendonitis causes pain on the front of the shin bone, usually at the lower aspect of the shin, closer to the ankle (lower 1/3). Walking, jumping or running can be painful, and symptoms should ease when stopping the activity.
It is often painful and stiff when stepping out of bed in the morning and eases within 5-10 minutes of walking. It may be painful at the start of exercises and then ease as it warms up but painful once again in the hour post exercises.
Chronic Anterior Tibial Tendonitis can be continuously painful with activity and increase in pain with continued use rather than easing.
There is rarely any bruising or discolouring, while there may be some mild swelling at the lower shin. It can be tender to touch along the Tibialis Anterior muscle, tendon, and shin bone. It is often confused with shin splints, but this condition is isolated to the tendon only.
Tibialis Anterior Tendonitis: Diagnosis
If you have any symptoms of Tibialis Anterior Tendonitis, it is recommended to have a consultation with a medical professional such as a Physical Therapist.
A clinician may resist active ankle dorsiflexion with pain along the Anterior Tibialis tendon indicative of a positive test. At the same time, we expect pain on palpation of the affected tendon.
A scan may be required to complement a clinical diagnosis. The most accurate scans for Anterior Tibial Tendonitis are an Ultrasound Scan or an MRI. An x-ray can rule out other conditions with similar symptoms, such as a Stress Fracture but cannot diagnose Anterior Tibial Tendonitis.

How to treat Anterior Tibial Tendonitis
Physical Therapy is the best form of treatment for Anterior Tibial Tendonitis. Initial home treatment can involve icing the area for pain relief for 10-15 minutes,2-3 times daily. Consider reducing impact activity to manage pain levels by 20-30% until your pain levels are stable. Nonsteroidal anti-inflammatories such as Ibuprofen can be helpful but should be guided by your GP. Foam rolling the Anterior Tibial muscle and stretching the calf muscle is helpful, too.
A physical therapist may carry out manual techniques such as soft tissue massage and assisted calf muscle stretching. An ankle brace or taping may be used in irritable cases for the tendon to settle. Common anecdotal treatments such as KT Tape and compression socks are of little clinical benefit for this condition.
Strengthening and stability exercises for the foot and ankle are recommended alongside stretching the Tibialis Anterior and calf muscles.
Gait analysis is recommended to assess for any biomechanical contributions to the pain. A custom insole may help control pronation forces when walking that can overload the Anterior Tibialis tendon.
In contrast, steroid injections such as cortisone are not recommended for tendon issues as they can cause long-term deconditioning of the tendon.
Surgery is rare, but a surgical tendon debridement may be required in persistent cases that fail conservative treatment. This is usually followed by 6-12 weeks of Physical Therapy.
Physiotherapy with James McCormack
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack. He offers Online Physiotherapy Appointments weekly.
Related Article: Extensor Tendonitis of the Foot

