Metatarsalgia Exercises
Read More >
The long bones in the forefoot are called metatarsals; the joint where they meet the toes is called the metatarsophalangeal joint. You can locate the metatarsophalangeal joint by lifting your toes and sliding your finger down towards the ball of the foot. You’ll find a slight hollow where the toe meets the metatarsal head; this is the location of Metatarsalgia.
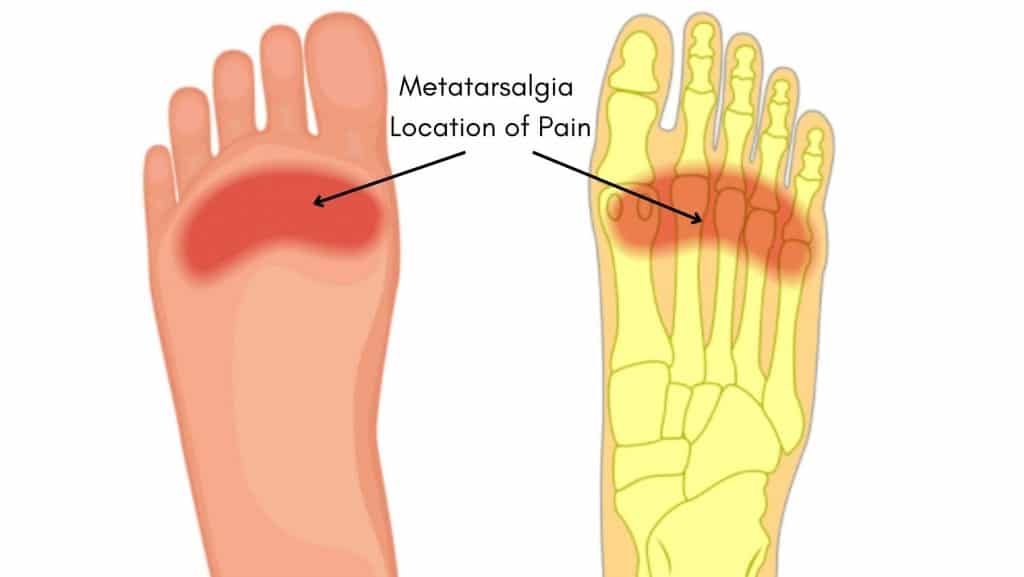
Metatarsalgia is a painful condition of the sole of the forefoot. Symptoms are worsened by standing, walking barefoot or in poor supporting footwear. Patients often describe a burning sensation on the underside of the foot at the base of the toes.
There may be numbness or tingling in the base of the foot, and patients sometimes describe the sensation of a pebble in their shoes, although this is more common in Morton’s Neuroma.
Other factors that irritate the symptoms of Metatarsalgia are walking on hard surfaces or impact activities such as skipping or running.
Several physiological factors and environmental factors can cause Metatarsaglia.
A Physical Therapist or a Sports Medicine Doctor is in the best position to diagnose Metatarsalgia. A clinical examination will examine whether any foot deformities may be causing your Metatarsalgia pain, such as Bunions, Tailors Bunions or Hallux Rigidus.
The clinician may occasionally refer you for imaging if they need assistance with a differential diagnosis.
An MRI is the gold standard scan for diagnosing Metatarsalgia. An ultrasound is a useful tool and a cost-effective solution for soft tissue structures of the ball of the foot but it is not as sensitive for bone injuries as an MRI while an x-ray is useful for diagnosing bone injuries such as a stress fracture but it can’t assess inflammation within the joint.

Metatarsalgia is primarily an inflammatory condition; in most cases, its symptoms can be eased with home treatment. While this is beneficial, it is important to address the causes. We discuss this later in the article.
The best home remedies for Metatarsalgia that we recommend to our patients are:
A Podiatrist or Physical Therapist is best placed to provide conservative treatment for Metatarsalgia.
As an inflammatory condition, the first stage of treatment involves a lifestyle discussion around reducing the time you spend on your feet and what you wear when you are active.
Cushioned trainers are often recommended, alongside a gel pad under the ball of the foot in the first instance. A gait analysis can sometimes reveal the necessity for insoles or custom orthotics, while a stability trainer may be sufficient otherwise.
An assessment may reveal muscular imbalances that can be improved with Metatarsalgia exercises. These can improve the foot’s balance, stability and mobility through strengthening exercises and stretches of the ankle and lower leg.

Other forms of treatment for short-term pain relief can include acupuncture, massage to the calf muscles and sole, compression socks, using a massage gun on the calf muscles and KT Tape.
If conservative treatment is unsuccessful, a referral for an ultrasound-guided steroid injection can be beneficial in reducing inflammation and pain within the metatarsophalangeal joint. This may be followed by 1-2 weeks in a walker boot for pain relief while allowing the injection to take maximum effect. Following this, continued conservative treatment is recommended.
In severe cases that fail conservative treatment, you may require surgery. Depending on the cause of pain, surgery can involve an elevatory osteotomy, a decompression osteotomy or a transpositional osteotomy.
In our experience, Metatarsalgia lasts up to 12 weeks. Still, suppose the symptoms of Metatarsalgia are identified in the early stages, and appropriate treatment under the guidance of a Physical Therapist is undertaken. In that case, Metatarsalgia can be resolved within 6 weeks.
In severe cases of Metatarsalgia, it can take 6 months to recover from Metatarsalgia entirely after conservative treatment and surgery.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Hallux Rigidus.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.