Best Shoes for Haglund’s Deformity
Read More >
A Haglund’s Deformity is a bony protrusion that develops on the back of the heel bone (Calcaneus). Sitting between the Calcaneus and the Achilles Tendon, as this bone growth develops, it can begin to rub off the back of the Achilles Tendon. It can lead to pain and inflammation in the tendon and the back of the ankle bone.
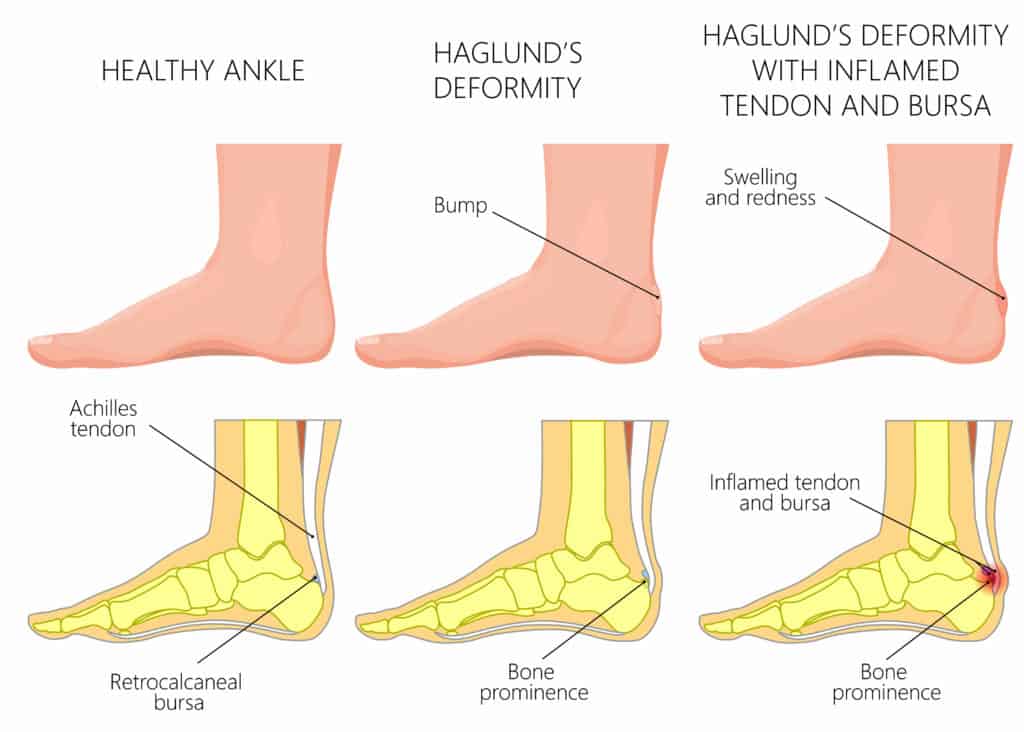
Haglund’s Deformity can cause pain and swelling on the back of the ankle when walking or if there is pressure directly on the deformity.
Patients report a burning and sharp sensation of pain that can be worse when walking uphill or running, while the most commonly observed symptom is pain when walking after rest.
A Haglund’s Deformity in isolation does not cause a typical pattern of stiffness in the morning that is associated with Achilles Tendonitis. Still, it is common to have both a Haglund’s Deformity and Achilles Tendonitis simultaneously.

Historically, the most common cause of Haglund’s Deformity is wearing tight-fitting shoes, previously known as ‘pump-bump’ from people wearing pumps.
There is some speculation that a tight Achilles Tendon can cause Haglund’s Deformity, but no concrete evidence exists to confirm this.
There is a mild genetic link but we speculate that wearing high heels or repeated friction on the back of the heel significantly contributes to its development.
A Physical Therapist or Sports Physical can quickly identify a Haglund’s Deformity from a clinical examination as it is associated with a large bump on the back of the heel bone alongside some swelling if it is particularly irritable.
Sometimes, a clinician may refer you for a scan to rule out other conditions, such as a calcaneus stress fracture. An X-ray is the easiest way to confirm the diagnosis, while an MRI may be requested to rule out any soft tissue involvement, such as Insertional Achilles Tendonitis.

Physical Therapy is the best form of treatment for Haglund’s Deformity. Following a physical examination, muscular imbalances that may be exacerbating your symptoms will be identified. A Therapist can create a thorough rehabilitation programme of stretches, strengthening and stability exercises to improve your foot and ankle control. This is essential for pain relief and reducing the risk of further symptom deterioration.
Orthotics and insoles are effective treatment methods for Haglund’s Deformity. Depending on your foot position and control, an off-the-shelf insole may be sufficient, or a custom-made insole may be required.
A conversation with your Physical Therapist about footwear options is an essential aspect of treatment, and a clinician who regularly treats foot and ankle conditions should be able to provide numerous footwear options.
An injection can be a suitable alternative in cases that fail to settle with Physical Therapy. A corticosteroid injection that is ultrasound guided is effective in reducing inflammation and pain levels. Depending on the severity of your symptoms, a period of 1-2 weeks in a walker boot may be recommended before recommencing Physical Therapy.
Surgery may be recommended if you try 6 months of conservative treatment and symptoms continue to impact your quality of life. Surgery can be in the form of an osteotomy or Gastrocnemius lengthening.
Yes, you can run with Haglund’s Deformity, as you likely have had the condition for a very long time. If you have Haglund’s Deformity without symptoms, you do not need to modify your running routine.
If you have mild symptoms during or after running, you should take steps to manage it with our suggested home treatment.
If you have severe symptoms, you can still run, but consider taking longer breaks between runs of up to 3 days, avoiding hill training and cross-training with cycling and swimming.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Haglund’s Deformity.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.