Achilles Tendonitis Exercises
Read More >
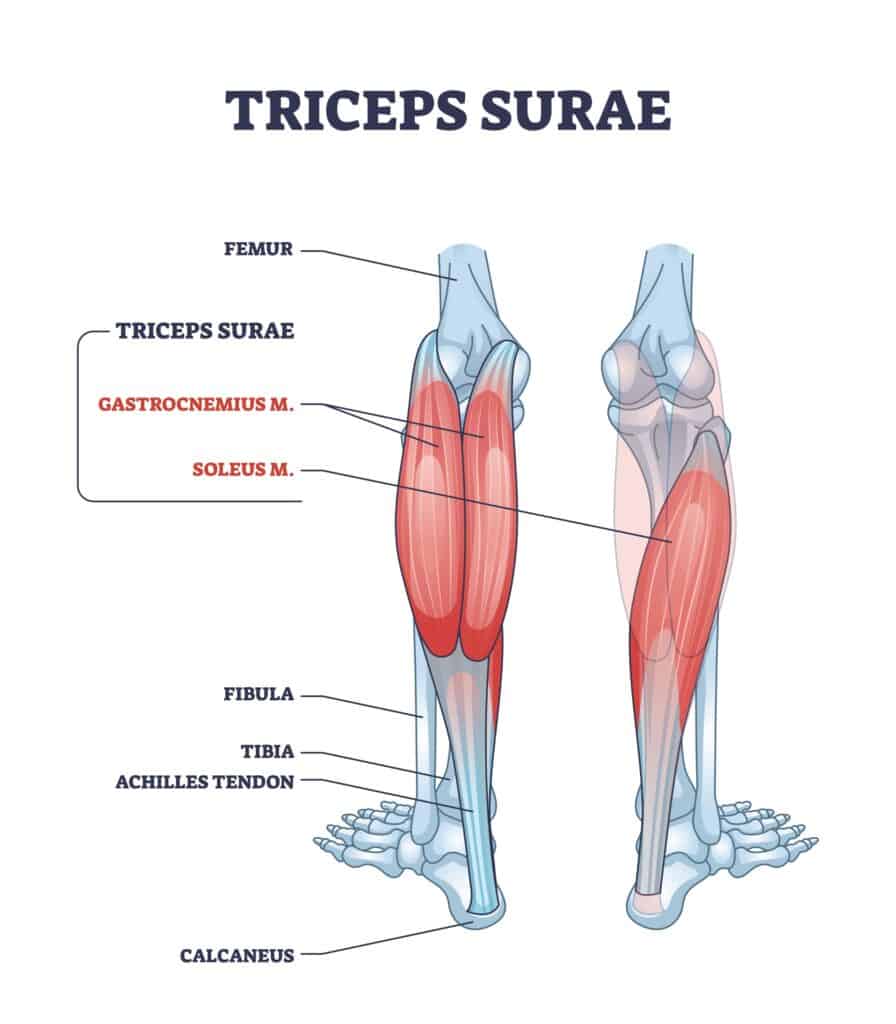
The Achilles Tendon is a long, thick band of fibrous tissue that connects the calf muscles to the heel bone. It is located at the back of the lower leg and is the strongest tendon in the human body. The tendon is made up of collagen fibres that are arranged in parallel bundles, giving it its strength and elasticity.
The Achilles Tendon connects the calf’s two muscles, the Gastrocnemius muscle and the Soleus muscle, onto the calcaneus bone (heel bone). The Soleus muscle is the larger of the two, and it is located deeper in the leg, originating from the soleal line on the dorsal surface of the tibia, medial border of the tibia, head of the fibula, and posterior border of the fibula.
A protective sheath surrounds the Achilles Tendon called the paratenon, which helps to reduce friction and protect the tendon from injury. The paratenon is a thin layer of connective tissue that covers the tendon and provides a smooth surface for the tendon to glide amongst the surrounding tissues.
The blood supply to the Achilles Tendon is limited compared to the calf muscles, particularly around its insertion into the heel bone. The reduced blood supply contributes to the Achilles Tendons’ notoriously slow recovery times. In addition, the tendon is subject to a lot of stress and strain, particularly during activities that involve running or jumping.
Common injuries to the Achilles Tendon include Tendinopathy (Tendonitis), Achilles Paratenonitis, and partial or complete tears. These injuries can be caused by overuse, trauma, or degeneration over time.
Understanding the Achilles Tendon’s anatomy can help prevent injury and enhance recovery. This article will explain the causes, diagnosis and treatment for Achilles Tendinopathy.
Based on a recent systematic review by the British Journal of Sports Medicine, risk factors for Achilles Tendinopathy include:
Numerous issues can cause Achilles tendon pain, and below we cover the most common symptoms for each. There is some debate regarding the level of inflammation in tendon pain issues. As a result, the term Achilles Tendonitis while still prevalent in the USA is more commonly referred to in the UK as Achilles Tendinopathy. As a result, we will use them interchangeably throughout the article.
An acute Achilles Tendinopathy is often the result of a sudden spike in activity levels that can cause constant and intense pain along the tendon, especially when it is placed under stretch.
This is often seen in the subacute phase of tendinopathy, where the pain is isolated to the middle of the Achilles Tendon only.
The most common symptom is stiffness in the morning on the Achilles Tendon that eases within 10 minutes of walking. There can be pain at the beginning of an activity, such as running, that eases during the run but is worse afterwards.
Insertional Achilles Tendon pain is located on the tendon’s attachment to the heel bone with no pain higher up the tendon.
Similarly to Mid-Portion Achilles Tendinopathy, it is common to have a stiff tendon in the morning with an Insertional Achilles Tendinopathy.
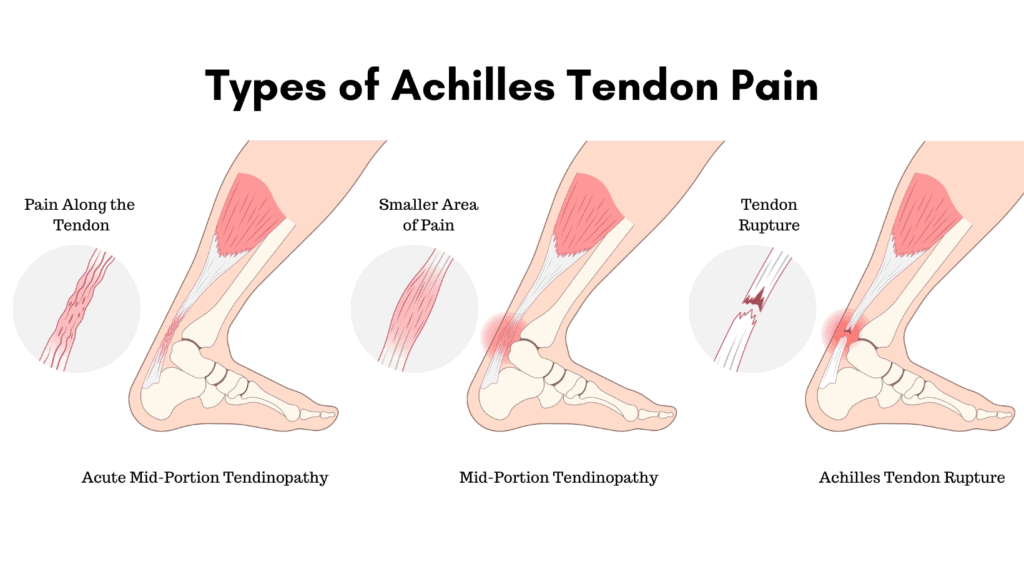
A torn Achilles Tendon differs from Achilles Tendinopathy as it is normally associated with a sudden onset of pain that causes a partial tear of Achilles fibres, whereas a tendinopathy is normally gradual in onset.
Someone may feel a sudden, sharp pain anywhere along the tendon when doing an activity. Other causes may be a Plantaris Tendon Tear.
An Achilles rupture is a complete tear of the fibres of the tendon. People often hear an audible pop or crack, describing the sensation of being kicked or hit with a small ball on their tendon.
Clinical examination by a medical professional involves palpating the tendon 2-6cm above its insertion to the heel bone. If there is pain, then the test is positive.
The Arc test has a sensitivity of 42% and a specificity of 88% in detecting midportion Achilles tendinopathy.
A Therapist will palpate along the tendon to identify a painful lump or swelling on the Achilles Tendon within 2-6 cm distal to the calcaneus. The clinicians pinches the lump/swelling and asks the patient to move their foot up and down. This test is positive if the examiner feels the nodule or swelling moving.
The Royal London Hospital test has been found to have a sensitivity of 54% and a specificity of 86%.
The examiner asks the patient to lie in a prone position with their foot off the edge of a bed. The clinician squeezes the tendon between 2-6cm distal to the tendon calcaneus insertion.
The patient dorsiflexes their foot, and the examiner pinches the same location. If the pain is absent, then the test is positive.

Thompson Test
The Thompson Test for Achilles Tendon Rupture has a sensitivity of 96% and specificity of 93%
The patient lies on their front (prone) with their knees extended and their foot relaxed and hanging over the edge of a bed. The examiner squeezes (compresses) the patient’s calf muscle, and if their foot doesn’t plantarflex, this is a positive test for a Tendon Rupture.
MRI and ultrasound scans are equally accurate (87%) in the diagnosis of Achilles tendon pain, but they should be performed alongside a clinical assessment. They are helpful for identifying thickening and inflammation within the tendon and paratenon.
An Ultrasound is usually the first option as it is cheaper and can be carried out in the clinic as part of an assessment.
X-rays are not used for Achilles Tendinitis are they can only detect bony injuries.

Strengthening Exercises are the single most effective form of treatment for Achilles Tendinopathy. There are two evidence-based rehabilitation protocols for Achilles Tendonitis: The Alfredson Protocol and the Heavy Slow Resistance Protocol.
Exercise Modification to reduce the amount of stress going through your Achilles tendon by reducing your daily step count and time on your feet. We do not recommend stopping running as this can decondition the tendon but consider reducing your running volume, increasing the gap between runs and performing non-impact activity.
Heel raises inside your shoes shorten your Achilles Tendon, and these are a medically proven form of pain relief from Achilles Tendinopathy.
Insoles for Achilles Tendonitis: There is moderately good evidence that insoles can reduce pain levels and facilitate rehabilitation by providing additional Achilles Tendon Support.
Achilles Tendon Taping, such as KT Tape, is common in clinical practice. There is little evidence to indicate its effectiveness.
Achilles Tendon Stretches for your calf muscles with a knee-to-wall stretch can elongate the calf muscle and provide short-term pain relief. There is also some evidence that stretching increases muscle cross-surface area, which may be why patients with Achilles Tendinopathy benefit from calf stretches.
An aircast walking boot may be advised if your Achilles Tendon is too painful to walk on.
Home Treatment for Achilles Tendinitis can provide short-term pain relief but is beneficial if you don’t have access to a Physical Therapist.
Icing the tendon for 10-15 minutes until the area is numb can relieve pain.
Anti-inflammatory use may benefit Insertional Achilles Tendinopathy, but there appears to be minimal to no benefit in using Non-steroidal Anti-inflammatories for Mid-Portion Achilles Tendinopathy.
Wearing a heeled boot or trainer takes the pressure off the Achilles Tendon.
Some patients find an Achilles Tendinopathy brace or night splint can help reduce morning pain and stiffness, but minimal evidence exists recommending its use.
GTN patches can be applied directly to the Achilles tendon and have been clinically shown to reduce Achilles Tendon Pain levels allowing you to stay physically active and improve outcomes from Achilles Tendon Strengthening Exercises.
Platelet-rich Plasma (PRP) is not recommended for treating Achilles Tendinopathy. Ultrasonography-Guided Corticosteroid Injection can help to reduce pain levels in Tendinopathy, but there is growing evidence that it can cause medium-term harm to the tendon.
There are very few instances where surgery is required for Achilles tendinopathy. In rare instances, Plantaris tendon issues can contribute to Achilles Tendon pain; in this instance, surgery could be beneficial.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack. He offers Online Physiotherapy Appointments weekly.
Related Article: Achilles Tendinopathy Exercises