Best MCL Knee Brace
Read More >
The MCL of the knee is the medial collateral ligament, attaching the femur and tibia on the inside of the knee. Ligaments are fibrous connective tissue that attach bones to bones and limit the movement of the joint in a particular direction. The MCL is made up of two parts, a superficial band and a deep band. Both are attached to the femur and the tibia but the deep band has additional attachments to the meniscus.
It is attached superiorly to the medial femoral condyle and inferiorly has two insertion points, one into the semimembranosus tendon (one of the hamstrings) and the second into the upper medial surface of the tibia.
It is divided into two: the meniscofemoral and meniscotibial ligaments. The meniscofemoral part attaches the femur to the medial meniscus, and the meniscotibial attaches the medial meniscus to the medial tibial plateaux.
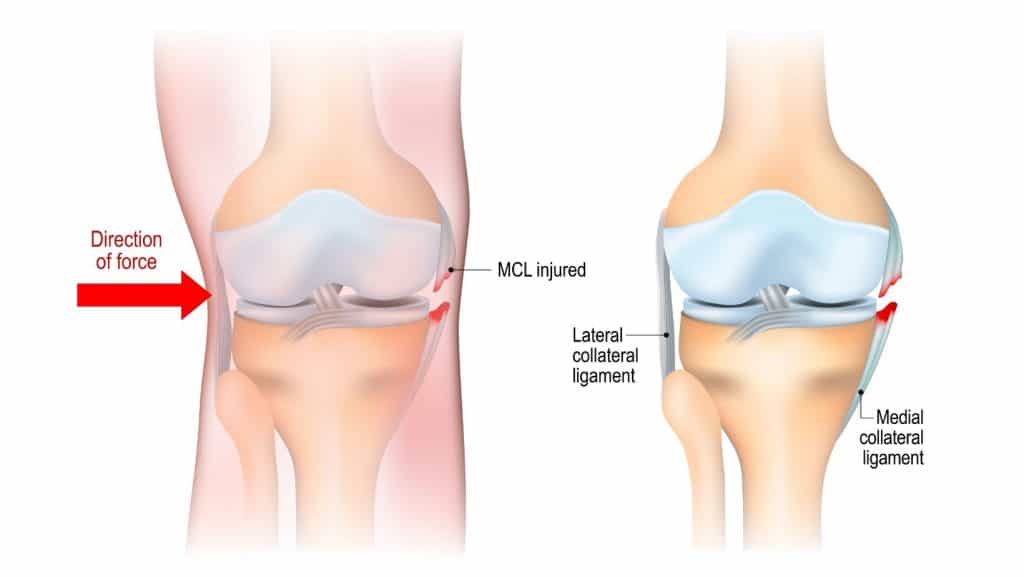
The primary function is to restrict the inward movement of the knee, known as a valgus movement. It also helps the smooth movement of the knee.
The superficial MCL also helps stabilise external rotation at 30º of knee flexion, and the deep MCL helps stabilise medial rotation when the knee is 0-90º flexed.
There is also some assistance in preventing hyperextension of the knee and the backward movement of the tibia on the femur.
An additional function is proprioception, which provides the brain with information about the joint position.

Injury occurs when the ligament is stretched beyond its capacity. The fibrous connective tissue is damaged as a result.
The most common mechanism of injury is an excessive inward force of the knee. This is commonly the cause of MCL injuries that occur from a fall, for example, when skiing, or with a tackle for example with rugby, football, or soccer.
Twisting the knee or hyperextension are other frequent mechanisms of injury. Jiu-jitsu and wrestling have a high prevalence of MCL injury.
Not all injuries occur through sport. A fall or direct blow to the area can cause damage to the ligament. And some people are more at risk than others.
If your knee moves inwards when walking, or if you are overweight, there will be more stress on the MCL, which can cause a chronic injury.
During pregnancy, hormones are released that make all ligaments more lax or stretchy, so during pregnancy, ligament injuries are more common.

The most common symptom is pain located on the inside of the knee. This may be more intense when bending the knee. MCL injuries vary depending on the grade, mechanism of injury and if any other structures were injured at the same time.
It might feel like an ache with a minor injury, more intense, sharp, or burning with more severe injuries. If there is a moderate to severe injury to the ligament, there may be bruising and swelling around the inside of the knee. But in many cases, there can be no swelling.
MCL injuries can present with symptoms that include instability or the knee giving way, and clicking or popping sensations. It may feel hard to bend or straighten the knee due to pain. Pain can be worse at night, and many people find it difficult to get comfortable to sleep.

It is essential to take a thorough history of symptoms, activity levels and if there was a specific mechanism of injury.
A knee examination should include a general assessment of the person’s joint mobility and strength, as well as specific orthopaedic tests. A valgus stress test is the best MCL injury test.
A valgus stress test assesses the laxity and pain of passively moving the knee into a valgus position with the knee at 0º and 30º of flexion. This can determine the grade of the injury.
Other tests should be performed to rule in or out of other possible diagnoses, which include: medial meniscus injury, Pes Anserine Bursitis and osteoarthritis.

Symptoms of low pain, without swelling or joint instability.
Minimal damage with less than 10% of ligament fibres torn.
Assessment will find pain on palpation of the ligament with 0-3mm of excess movement of the joint.
Symptoms of moderate to high pain, with swelling and very mild if any joint instability.
Moderate damage with more than 10% of ligament fibres torn.
Assessment will find pain on palpation and swelling, and there is 5-10mm of excess movement of the joint with pain.
Symptoms of high pain, with swelling and joint instability.
Severe damage with complete or near complete rupture of the ligament.
Assessment will find pain on palpation, swelling and >10mm of excess movement of the joint or no end feel to ligament stress tests, this may be accompanied by pain if the tear is not complete, or can be pain-free if completely ruptured.
In addition to clinical assessment, imaging with MRI, ultrasound and X-ray can be helpful to rule in the diagnosis of an MCL injury and rule out other conditions.
Sensitive imaging, such as MRI or ultrasound, can also help classify the injury.

The human body has a fantastic capacity to heal. A grade 1 MCL tear is likely to heal with no additional intervention, provided it is given adequate time to rest and recover. In a healthy person, this will usually take 1-3 weeks.
The greater the injury and level of damage the longer the healing will take and the more interventions will aid recovery. A grade 2 or 3 tear will benefit from restriction of movement. Both full extension and more than 90º knee flexion put more stress on the ligament and can delay healing.

An initial period of home treatment involves rest and ice, and if there is swelling, compression and elevation, for several days to a week.
No sport and minimal walking should be performed during this time. Exercises for joint mobility, muscle flexibility and activation of the quadriceps are helpful during this period.
If pain is high, crutches might be helpful for mobilising but are not often needed for this level of injury.
A biomechanical assessment is helpful once the pain has subsided to see movement quality and address tight or weak areas that may have contributed to the injury or impact recovery. Building strength in the leg muscles around the knee joint will help support the knee.
Recovery from a grade 1 MCL injury is between 1-4 weeks.
The initial rest period of 2-4 weeks should include the use of a brace, and in most cases for grade 2 tears and all cases of grade 3 tears, crutches will be needed to reduce weight bearing and manage pain.
Ice and medication can be used for pain relief, and compression and elevation are strongly recommended as there will be swelling.
Rehabilitation should be guided by a medical professional such as a physical therapist. Rehab protocols include early activation exercises for the quadriceps muscles to facilitate faster recovery. You can read more about exercises in our article, MCL Injury Exercises.
Recovery from a grade 2 MCL injury is between 4-8 weeks and from a grade 3 MCL injury is between 8-12 weeks but can take longer if surgery is required.

It is expected to have difficulty finding a comfortable sleeping position with an MCL injury. Either pressure on the inside of your knee or your knee being entirely straight can be painful. Here are some tips to help you get comfortable and get a good night’s sleep.
Sleeping on your side: place a pillow between your knees to keep your knees hip-width apart and provide some cushioning from the pressure of your knees together.
Sleeping on your front: place a pillow under your ankles to keep your knees slightly bent and lessen the pressure on the front of your knee.
Sleeping on your back: place a pillow under your knees to keep your knees slightly bent and supported.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Knee Pain.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.