Knee Pain Location Chart
Read More >
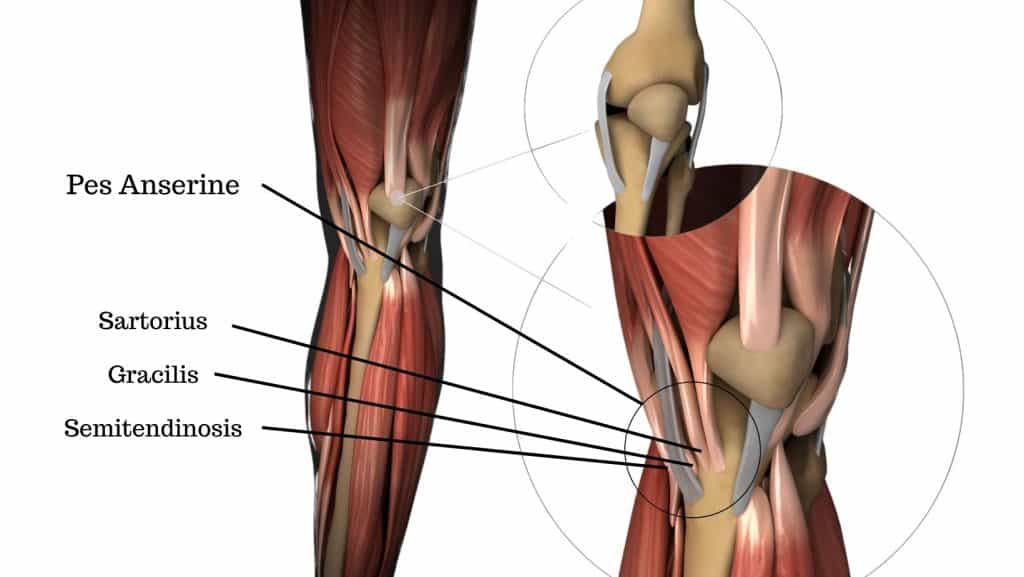
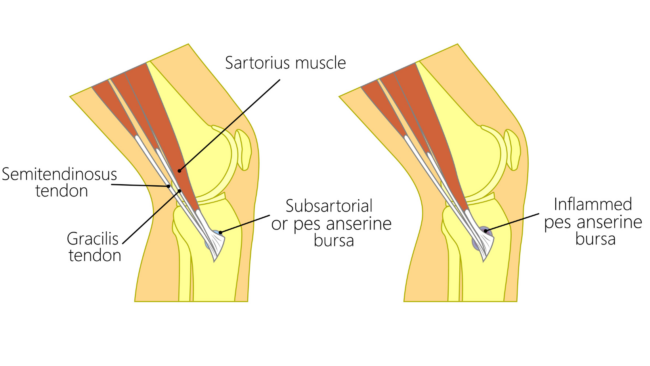
The pes anserine is the combined insertion point of 3 tendons at the inside of the knee. The attachment point is just below the knee on the inside of the tibia bone. The tendons are protected by a bursa that is situated between the tendons and the bone. Inflammation of the bursa causes pes anserine bursitis.
The term ‘Pes Anserine’ is Latin for ‘Goose Foot’, named because of its appearance.
The 3 tendons that form the pes anserine are the sartorius, gracilis and semitendinosus. These muscles have several different actions: to flex the hip, abduct the hip, adduct the hip, external rotation of the hip, and flex the knee.
A bursa is a thin membrane sack, similar to a deflated balloon. It contains a small amount of fluid to provide lubrication. It can therefore slide easily to relieve friction between moving parts.
Pain: felt on the inside of the knee, usually just below the joint on the inside of the shin bone. Medial joint line pain is also commonly reported. Pain is often described as an ache. Occasionally, more intense with specific movements that compress the bursa. It may feel sore or burning-type pain.
Inflammation: the skin can appear red and feel hot to the touch. It can also appear as a swollen lump in this area.

Pes anserine bursitis symptoms can develop gradually over time due to repeated overload. But it can begin suddenly if the injury is related to trauma or a direct impact.
In most cases, it will develop at one knee, but it is occasionally present in both knees.
Pain can be aggravated by exercise but worsen after. Commonly taking over 24 hours to settle down.
There are two main causes of Pes anserine bursitis, traumatic or chronic overload:
Traumatic injury to the Pes Anserine bursa occurs when there is a direct impact on the bursa. This may be from a tackle in sport or simply from knocking your knee on something.
The more common cause of Pes Anserine Bursitis is the result of chronic overload. Usually related to an individual’s biomechanics. It may be triggered by an increase in an activity, such as walking or running. Knee valgus (see image) and flat feet are common biomechanics seen with this condition.
Other risk factors include diabetes, obesity and osteoarthritis of the knee. Women are more likely to get this condition than men, with a greater risk over 50 years old.
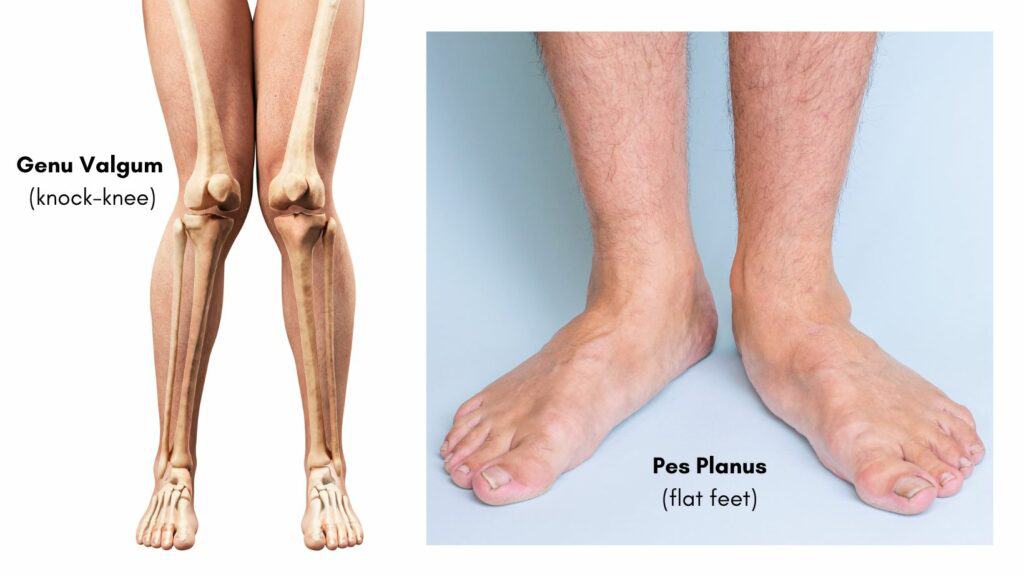

Pes anserine bursitis is also very common in runners, as running is a repetitive, high-impact sport. Therefore, it requires a high level of strength and endurance to prevent inward movement of the knee.
The repeated overload of the bursa through running will often develop following an increase or change, such as increasing distance, frequency, speed or terrain.
A diagnosis of pes anserine bursitis is made from a combination of the history of onset, symptoms, and activity, as well as a physical examination and clinical tests.
The examination will include applying pressure over the pes anserine bursa, which will be sore if it is inflamed. Resisting the action or stretching the 3 muscles that insert at the pes anserine, can also trigger symptoms. A biomechanical or gait assessment can reveal risk factors.
Clinical tests to rule out other pathologies and causes of pain inside the knee, such as the meniscus, medial collateral ligaments and saphenous nerve, help confirm the diagnosis.

There is no specific pes anserine bursitis test. Therefore, radiology can be used to confirm a clinical diagnosis. MRI is the best form of imaging to get an accurate diagnosis.
Pes anserine bursitis responds well to treatment. A physical therapist will be able to guide and tailor a treatment and management plan that is specific to you.
The typical healing time for pes anserine is 6-8 weeks. Factors that affect healing time include specific biomechanics, health and underlying conditions, and compliance with rehabilitation.

Physical therapy may include massage, joint manipulations, acupuncture or dry needling and most importantly rehabilitation exercises.
A specific programme of stretches and rehabilitation exercises will be prescribed based on your biomechanical assessment.
Pes anserine bursitis recovery can be aided with the use of tape. Either ridged tape or elasticated tape such as Kinesio tape can be applied to the knee. The aim of tape can be to offload pressure from the pes anserine bursa and to increase awareness of poor movements to help correct these.

For pain relief using ice directly over the bursa is very effective. Heat over the inflamed bursa can make it more painful but it can be used over the muscles further up the inner thigh to assist with relaxation if they feel very tight.
As pes anserine bursitis is an inflammatory condition, anti-inflammatory medications can be effective.
In cases where symptoms do not settle a cortisone injection into the bursa can be helpful. This reduces the inflammation of the bursa and can break the cycle of pain and irritation.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Knee Pain.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.