Patellar Tendonitis (Jumper’s Knee)
Read More >
The quadriceps muscles group comprises the Vastus Lateralis, Vastus Medialis, Vastus Intermedius and Rectus Femoris. Therefore, sometimes, this tendinopathy is called rectus femoris tendonitis or quadriceps femoris tendonitis.
Quadriceps tendonitis results from an overload or overuse of the quadriceps tendon. Overload without adequate recovery time for the tendon to strengthen and adapt, will cause degeneration in the tendon. Tendonitis can also been known as a tendinopathy.
The quadriceps is the primary muscle group to straighten the knee. It is, therefore, used for many activities such as walking, running, jumping and squatting.
Participating in sports that incorporate these movements with high force, speed or repetition, such as basketball or volleyball, will mean it is more likely to develop this condition. These sports require powerful contraction of the quadriceps to create the force to jump or sprint. Hence, this injury is often referred to as Jumper’s knee.

Tendonitis can be caused by an acute or chronic overload. Acute cases will be triggered by a sudden increase in load or a direct impact on the area.
Commonly, this will be the impact from a fall on the knee or being hit by a ball or bat. Pain will start suddenly at that time or very soon after. A rapid increase in volume of a specific activity or training, such as jumping or sprinting, can also trigger this.
Chronic cases will develop more gradually over a period of time. This can be over a period of weeks or months of overload without adequate recovery time. Pain will develop slowly from a slight discomfort and will worsen if the overload is continued. If pain persists for 3 or more months, this can be described as chronic quadriceps tendonitis.

In this sporting population, more men compared to women develop quadriceps tendinopathy. Younger age, greater height and weight, as well as greater volumes of strength and jumping training also increase risk.
Biomechanics that can increase risk include excessive knee bend when walking or running, overpronation and poor foot posture, and valgus knees.
In the non-athletic community, quadriceps tendonitis also exists. Activities such as kneeling can also overload this area. Some medical conditions can also change tendon structure and load capacity.
Scientific research shows that people with diabetes are three times more at risk of musculoskeletal conditions, in particular tendon pain. They are also less likely to respond well to treatment.
Obesity is a growing problem and also shows a higher risk of tendonitis, tear and rupture in research. These individuals are also more likely to have complications from tendon surgery.
This is due to higher levels of inflammatory proteins than non-obese individuals and the greater mechanical load on the joints. Obesity is also associated with the development of type 2 diabetes.

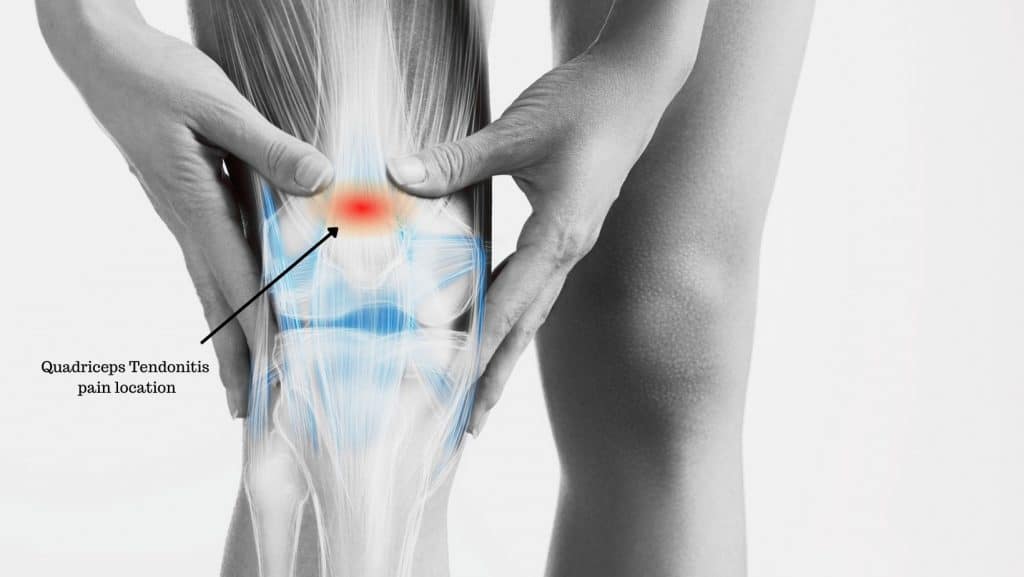
In most cases, there is a gradual onset of pain or discomfort at the front of the knee. Pain is usually most significant at the insertion of the tendon to the bone at the top of the patella. But can be felt up into the low and mid part of the thigh, in the main part of the quadriceps muscle.
The pain of quadriceps tendonitis is usually described as a soreness or ache. In severe as well as acute cases pain can be extreme, sharp, or burning.
Secondary to the pain, many people report knee stiffness, and a tight quadriceps muscle. It is often described as feeling difficult to bend the knee. Some people also feel and hear a cracking or popping sensation when they bend and straighten their knees.
Occasionally, there can be swelling around the attachment area of the tendon to the patella. Swelling is usually very focal and not diffuse over the whole knee.
In the initial stages and milder cases, the pain will be intermittent. Symptoms are usually felt first thing in the morning or after exercise and activities that aggravate the tendon. There is often a delay of a few hours. Pain can last for a few hours or days, before easing off, if the area is rested.
In severe cases or if aggravating activities are continued, the pain will become continuous. Careful monitoring of the pain or the keeping of a pain diary can help identify patterns. This can indicate which activities might be aggravating the pain.

A clinical diagnosis is made with a physical assessment of the knee. Common symptom patterns and clinical tests can indicate patella tendinopathy.
Importantly, clinical assessment must also rule out other causes of anterior knee pain. Other common causes including PJF Syndrome, Fat Pad Syndrome and Patella Tendonitis.
It is uncommon for there to be locking, giving way, or diffuse swelling around the knee joint. And unless there has been a direct impact, bruising is rare. These symptoms may indicate a different diagnosis.
In some cases, radiology is used to confirm the diagnosis. MRI and diagnostic ultrasound are the most accurate.
Both will show swelling and inflammation, bursitis, collagen breakdown, development of new blood vessels or calcific changes. These are all physiological changes that are signs of tendonitis.
X-ray imaging is less sensitive, and many of these changes will not be seen, but it can be helpful to rule out conditions such as arthritis.

Quadriceps tendonitis treatment should start as soon as symptoms are first experienced.
Physiotherapy for quadriceps tendonitis is very effective. Physiotherapists are experts in soft tissue injuries and will guide treatment and educate you about the injury. The most up-to-date and relevant treatment for tendon pain is P.E.A.C.E. and L.O.V.E.
The initial phase is P.E.A.C.E: P =Protect, E = Elevate, A = Avoid non-steroidal anti-inflammatories (such as ibuprofen), C = Compress, E = Educate the individual about the injury.
The next phase is L.O.V.E: L = Load, O = Optimism (a positive outlook has been shown to improve outcomes), V = Vascularisation (increase blood flow with non-aggravating exercise), E = Exercise (specific strength and conditioning for the tendon).
We have written a separate article about rehabilitation exercises. In addition to education and rehabilitation exercises, physiotherapists can offer different treatments to help promote your recovery.

Acupuncture or dry needling, is effective for pain relief and improving function and can aid healing from tendonitis. Acupuncture works by increasing the synthesis of type 1 collagen, which is necessary for the repair of tendons, and this type of collagen positively influences the biomechanical properties of a tendon.
Massage and trigger point release can be effective for pain relief and can help reduce the strain on a tendon. This can occur if the surrounding muscles are tight. You can also perform massage on yourself.
The primary use of taping during quadriceps tendonitis treatment is pain relief. In most cases by lifting the patella to offload the tendon.
There is poor scientific evidence about the efficacy of taping. but it is low-cost and safe. As many people report a perceived benefit, it can be worth trying.

One taping technique is elasticated sports tape, called Kinesio tape, KT tape, or Rock tape.
Another option is using ridged tape, often called zinc oxide tape, which is not elastic. Clinically, we have found this taping method to provide more pain relief for patients.
Knee braces and compressive sleeves can be worn for quadriceps tendonitis. The main function of a brace is to offer support for the joint and compression.
Compression can help in two ways. It can help by reabsorbing swelling and reducing stagnation. And it can help by providing greater proprioception of the area.

GTN patches are glyceryl trinitrate or nitroglycerin patches that can be applied to the skin over the tendon. The compound is absorbed through the skin and reduces pain in the tendon. It is thought that it helps by dilating blood vessels and may stimulate collagen, which aids the healing process of the tendon.
Shockwave Therapy potentially works in three different ways: by shocking the nerves and reducing their conduction, therefore reducing pain; affecting specific properties of cells during the recovery process; and by breaking down calcium deposits that develop in poorly healed tendons.

A more invasive treatment is an injection. Corticosteroids are used for the anti-inflammatory effect. There is some evidence to show that there can be a negative effect on the structural integrity of the tendon.
Therefore, this treatment is done with caution. If it is used, there will be a limit to the number and frequency of the injections administered to the tendon.
Surgery is a last resort once all other treatments have been tried for a period of 3-6 months without a satisfactory recovery. Traditional surgery includes the removal of diseased portions of the tendon or calcification that can form with tendonitis.
A recent development with surgery is using a scraping technique that removes the small nerves that can form. The outcome of this new technique is more favourable regarding pain reduction. There is also a quicker return to sports and activities post-surgery.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Quadriceps Tendonitis.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.