IT Band Exercises
Read More >
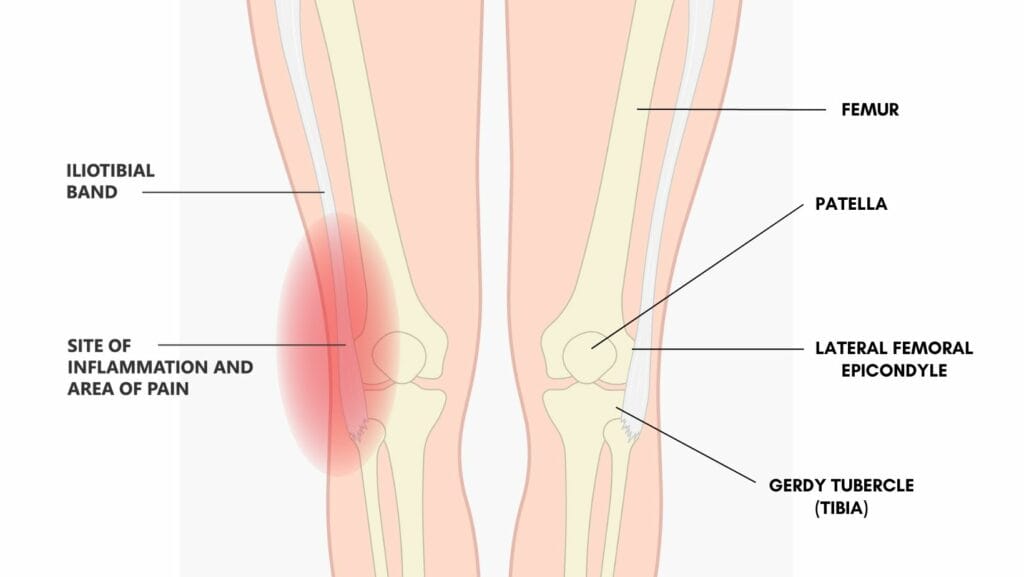
Iliotibial band syndrome presents with pain at the outside of the knee. It can affect one side or both. Some people additionally feel lateral hip pain, thigh or quad pain, and, less often, shin pain.
The most common site of pain is the outside of the knee because of where the IT band moves over a bony prominence. The most compression is when the knee is bent or straightened through 20-30º. Usually, at this angle, symptoms are most severe.
Unfortunately, we can move our knees through this range when walking, running, cycling or driving. So this condition can be very debilitating. Many people find the pain so high they are unable to run through it. In extreme cases, you may be unable to walk without aggravation.
Symptoms are usually described as a dull ache, that can become sharp or burning with some positions or actions. Worse pain can be with lying on your side and it is common to feel pain at night.

The iliotibial band is a strip of connective tissue band running down the outside of the leg. Originating from the outside of the iliac crest, the top of our pelvis, it inserts at its lowest point to the tibia, our shin bone.
The iliotibial band has connections into multiple bones and muscles down the outside of the leg:
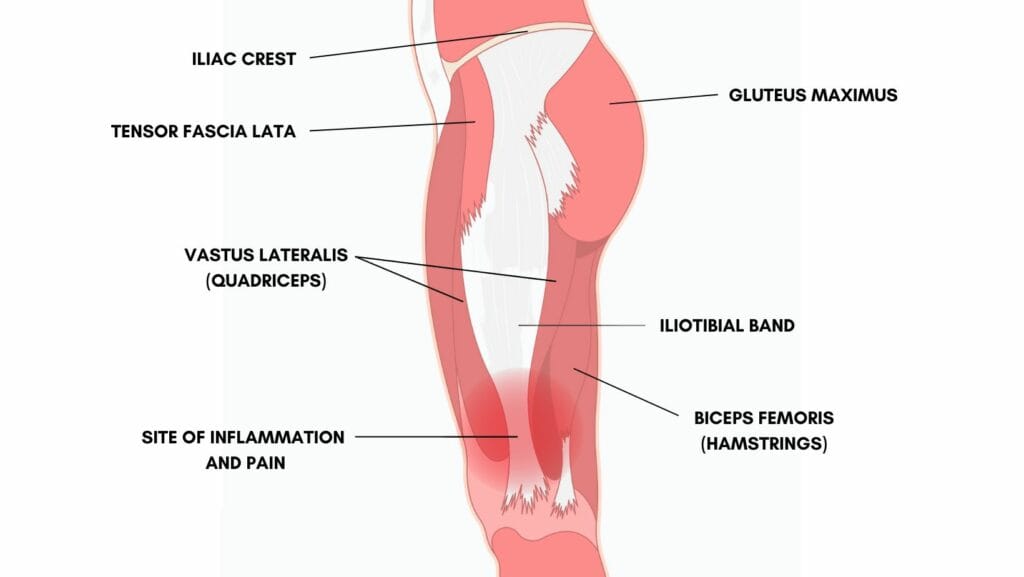
The iliotibial band stabilises the pelvis and controls posture. It does this by assisting with hip extension, abduction, and external rotation.
At the knee, the IT band can assist with knee extension when the knee is slightly flexed (less than 20-30º) and assist with knee flexion when the knee is more flexed (more than 20-30º).
The iliotibial band regularly moves over the lateral femoral epicondyle. It is in front of this epicondyle when the knee is less than 20-30º flexed and behind it when it is more than 20-30º flexed.
A physical therapist or sports doctor will clinically assess your injury. A subjective assessment will highlight specific mechanisms of injury, such as trauma or a relevant training error. A physical examination will look at biomechanics, strength, flexibility, and specific diagnosis tests.
Diagnostic tests put the IT band under tension and compress the underlying fat pad. Ober’s test and Noble’s Compression test are the most commonly used. Pain on stretch and application of compression represents a positive test.
Radiology can confirm a clinical diagnosis. MRI scans and ultrasound imaging are accurate and effective. Both can show inflammation and swelling of the iliotibial band and underlying fat pad. X-ray does not show valuable information.

Other conditions can present with similar symptoms: Trochanteric bursitis, Pes Anserine bursitis, or a meniscus tear. It is important to have an assessment with an experienced clinician to get the correct diagnosis and, therefore, a correct management plan.
The repetitive movement of soft tissue over the hard bone is protected by a fat pad to prevent injury. The persistent compression and irritation of this fat pad results in iliotibial band syndrome. The fat pad is the painful part rather than the iliotibial band.
Specific specific biomechanics can increase the injury risk. These include flat feet, poor hip or knee control, hypermobility and a narrow running gait. Learn more about the functional anatomy of the iliotibial band in this paper.
ITB syndrome is very common in runners especially as individuals increase distance. Marathon training is a common cause of IT band pain as many people underestimate the time needed to condition their bodies. Common training errors are:

The biomechanics, or style of your running can also affect your risk of ITB pain:
Other sports that can cause ITB pain are cycling, long-distance walking, and golf.
These sports have the significant repetition of bending of the knee through the provocative range of 20-30º of knee bend, which can result in irritation of the ITB and underlying fat pad.

Outside of sports, ITB syndrome is common in people who are overweight. The additional weight on the joints, especially if accompanied by poor strength, puts this group at risk. Similarly, pregnant women are at higher risk due to the increase in laxity of the ligaments as a result of hormone changes and increased weight.
The reduction of strength in the elderly puts them at a greater risk. After knee or hip replacement, the reduction of strength, as well as the change of biomechanics, can also trigger the onset of ITB pain.
Initially, it is important to seek an experienced professional to assess your injury and they will provide the best plan of action specific to you. Typically complete rest or significant reduction of activities that aggravate pain will be necessary for ITB syndrome.

Treatment and exercises will initially focus on flexibility. Massage, stretching and foam rolling areas that are tight can reduce pain significantly.
Strengthening exercises for weak areas can take more time to have a noticeable effect but is the long-term solution for most cases. Read more about exercises for the recovery and prevention of iliotibial band syndrome in our IT Band Exercises article.
IT band taping is an effective short-term aid for pain relief, perceived stability and improving biomechanics. It is often used to get through a competition or event. This should not be used instead of addressing the problem.
Using rigid or KT tape can help with stability at the knee and reduce the compression of the sensitive fat pad, thus reducing pain. This video shows how to apply KT tape for iliotibial band pain.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Knee Pain.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.