Patellofemoral Pain Syndrome (Runners Knee)
Read More >
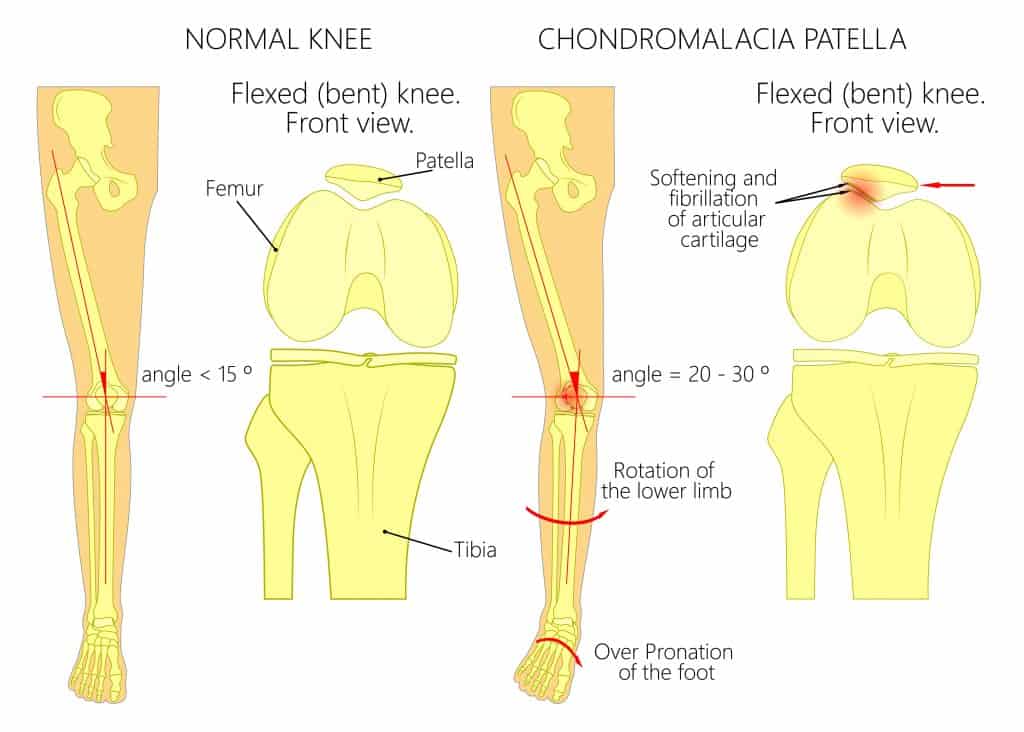
Chondromalacia Patella is the deterioration and softening of the cartilage at the back of the patella.
“Chondro” in chondrosis means relating to cartilage. “Osis” means relating to a pathological state. Chondrosis is therefore the pathological state of cartilage. It is a general term used to describe the softening and breakdown of the cartilage at a joint. This term can be used for any joint in the body. It is more common in certain joints than others, such as the knee, hands, hips, neck and lower back.
Chondromalacia Patella is the specific term for chondrosis of the retropatella cartilage. It is a degenerative joint disease that can be acute or chronic. Classification is based on the severity of degeneration of the cartilage surfaces, there are 4 chondromalacia grades.
Yes. This process also is commonly called patella or patellofemroal osteoarthritis.
The earliest stage of articular cartilage damage. Damage occurs to the surface of the cartilage and it starts to soften.
A progression of the articular cartilage damage. The softened cartilage will start to develop pitting and fissuring on the surface.
A further progression of the articular cartilage damage. The softened cartilage is damaged with pitting and fissuring reaching down to the bone.
The most severe articular cartilage damage. There is extensive damage and complete wear of the cartilage surface to expose the underlying bone.


Chondromalacia patella and patellofemoral joint pain are more common in women than men, and most common in the age group 50-59 years old. Greater weight and obesity increase risk, as do some biomechanical factors such as a high Q angle where the knee moves inwards.
Hypermobility conditions such as Ehlers-Danlos Syndrome often have issues with maltracking of the patella which increases the chance of damage to the retropatella surface.
In addition to these risk factors, trauma and injury such as a fall on the knee can cause injury to the cartilage of the patella.
Clinical assessment is the basis for a sound diagnosis. The history of the onset of symptoms or the mechanism of injury will be discussed. The pattern of symptoms and a medical history taken.
The practitioner will want to get an understanding of the individual’s level of activity and if there have been any changes to their exercise and daily routines that might have contributed to the onset of their condition.
A physical examination will look at flexibility, strength and biomechanics, as well as specific tests to see if symptoms can be reproduced. The McConnell test for chondromalacia patella is described below. A clinical diagnosis can also be supported by the use of radiological imaging.

With the patient sitting with the femur externally rotated and the knee flexed to 120º, the patient contracts the quadriceps isometrically for 10 seconds. If pain is experienced the knee is passively straightened by the clinician.
The contraction is repeated with a medial glide to the patella. If the pain is less with the medial glide then the probability of chondromalacia patella is increased. To be thorough, the test can be repeated at 90º, 60º, 30º and 0º of knee flexion.
Radiology of choice for grading of diagnosis
Will show subchondral oedema
Will show extent of pitting and fissuring to the cartilage surface
X-ray findings of reduced cartilage thickness
Will show bone-on-bone contact

Before considering the best treatments, it is essential to know what you already do that can aggravate your symptoms. Running and other high-impact exercises can irritate the patellofemoral joint as it has to withstand high compressive forces with each stride, lunge or jump.
It may not be a sport that makes the knee pain worse. Activities such as walking, ascending or descending stairs, or prolonged sitting with knees bent can all be aggravators. Alterations in your activities and habits are necessary to reduce inflammation and pain. It is good to have a period of reducing pain before starting rehabilitation.
A period of complete rest may be necessary for some people. Relative rest will be adequate for others, where activities that aggravate symptoms are significantly reduced in terms of duration, frequency or intensity.


A physical therapist can guide chondromalacia patella treatment. Your specific biomechanics might contribute to the development of chondromalacia patella or affect your recovery.
Common biomechanical issues are:
You can read more about valuable exercises for these biomechanical contributing factors in our related article: Chondromalacia Patella Exercises.
As well as rehabilitation exercises, a physical therapist can help to reduce symptoms in the acute phases with hands-on treatments. Massage can relax muscles such as the quadriceps, and patella gliding exercises can help mobilise the kneecap.
A knee brace or compressive sleeve will not fix chondromalacia patella but can help with proprioception and might offer some symptom relief.
Our recommendation for the best knee braces for patellar chondromalacia are those that:


With a correct diagnosis, appropriate rest from aggravating activities, and a specific exercise programme, most people will feel a reduction or resolution of their symptoms within 4-6 weeks. The level of improvement will depend on the severity and duration of symptoms and the grade of chondromalacia damage.
In most cases, it is continuing rehabilitation exercises at home for several months after physical therapy treatment is advisable. If the level of damage is moderate to severe, a maintenance programme of exercises will be necessary to continue on a long-term basis.
You can continue to walk with Chondromalacia patella depending on the severity and duration of your pain.
If you only get your pain related to higher impact or intensity sports, walking might be okay to continue unlimitedly (within reason). Specifics such as walking down hills or steps may be more aggravating than on the flat, and footwear can play an important role.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating knee pain.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.