Patella Fracture
Read More >
Tibial plateau fractures are relatively rare, accounting for only 1-2% of all fractures. The majority will fall into two main categories of the mechanism of injury, either a high-energy injury in the younger athletic population or a low-energy injury in an older population in combination with osteopenia or osteoporosis. It is a serious injury that can have complications of nonunion of the bone, infection as well as loss of range of motion of the knee joint, and the development of posttraumatic arthritis.
The tibial plateau is a broad and flat area at the top of the tibia which is the lower surface of the knee joint. It comprises of a medial and a lateral plateau, separated by the intercondylar eminence in the middle. These are weight-bearing areas of the knee that can be injured with high force in a vertical direction as the knee flexes, or a vertical force if the knee is in a valgus or varus position, which means either a knocked-knee or bowed-knee posture.
A high-energy injury such as a tibial plateau fracture will often also cause additional injury to the surrounding tissues of the knee, such as ligaments and the meniscus. You can read more about these injuries in our related articles: ACL Sprain, PCL Tear, MCL Injury, and Torn Meniscus Recovery.
Classification of this injury is helpful for several different reasons, not only for the prognosis of the injury and to guide treatment but also to communicate clearly with the patient and medical professionals, and for research. The tibial plateaux fracture classification by Schatzker is widely used (Berkson and Virkus, 2009).
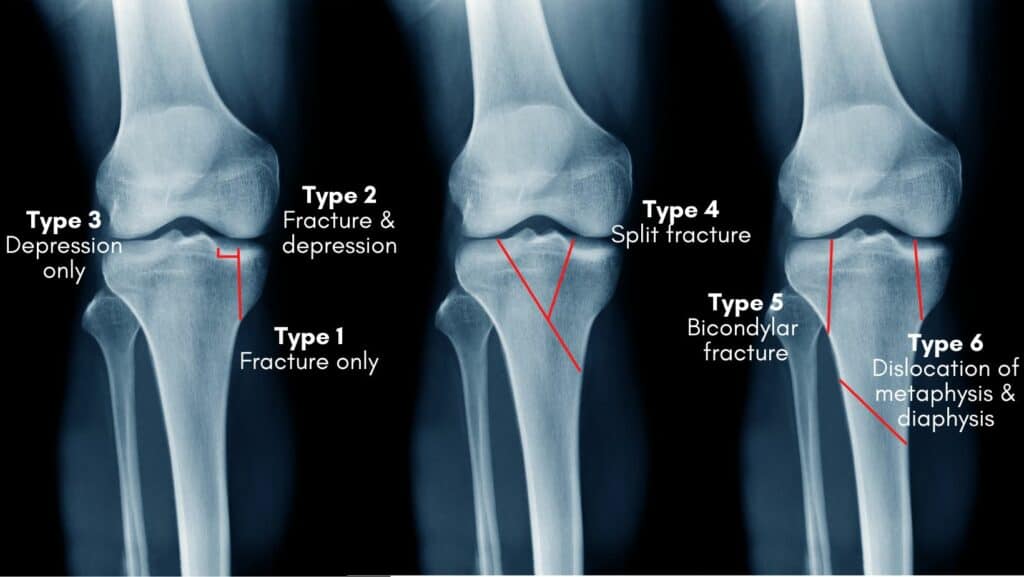
Lateral split and depressed fracture.
This is a cleavage and compression fracture, with a depression in the lateral plateau of more than 4mm. This is the most common type.
Central depressed fracture.
This is a depression fracture with no cleavage fracture, it can be either a lateral depression (type 3a) or a central depression (type 3b).
Split fracture.
This is a fracture of the medial plateau with or without a depression fracture and has a poor prognosis.
Bicondylar fracture.
The spine of the tibia is continuous with the shaft with fractures on either side to the medial and lateral condyles.
Dislocation of metaphysis and diaphysis.
This is a complex fracture of the medial and lateral condyles and to the shaft of the tibia.
A tibial plateau fracture will present with significant to severe knee pain with swelling and bruising. The patient will feel unable to weight bear due to pain and if does weight bear will feel unstable. The range of movement of the knee will be reduced in both flexion and extension.
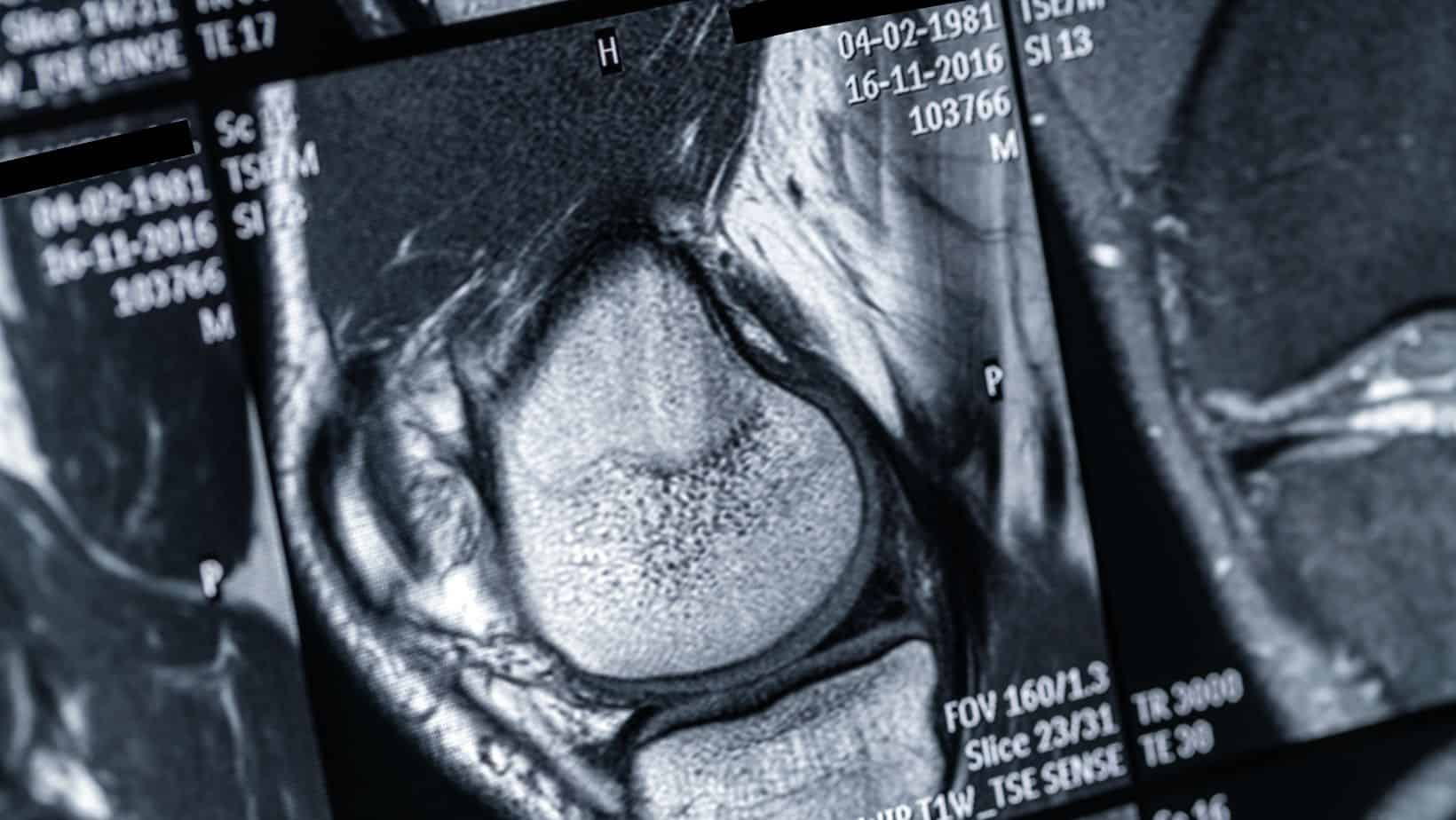
Diagnosis is confirmed via radiological imaging if there is suspicion of this injury from clinical examination. MRI will provide the most information on the fracture and concurrent soft tissue injuries, which are likely. Ligament, muscular and cartilage injuries are likely.

Tibial plateau fractures can be conservatively managed if the fracture is stable and joint alignment is good. Additionally if the patient is elderly, in poor health or has a high risk of infection. These cases can be managed well with casting or braces and a period, and usually a period on non-weight bearing to allow the fracture to heal.
Surgical management is advised if the fracture is unstable or displaced, and for younger and more active patients. The bone will be stabilised with screws and plates, and in some cases bone graft of bone cement is needed.
Most patients who are fit and healthy recover well from a tibial plateaux fracture, if well managed and if advice is adhered to. After surgery, for example, most people are comfortable and able to start returning to weight-bearing and walking 6 weeks after surgery and will be returning to sports and higher-impact activities after 4-6 months. If conservatively managed recovery time will be similar.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack. He offers Online Physiotherapy Appointments.
Related Articles:
Posterior Horn Medial Meniscus Tear
Lateral Meniscus Tear
MCL Injury