Posterior Tibial Tendonitis
Read More >
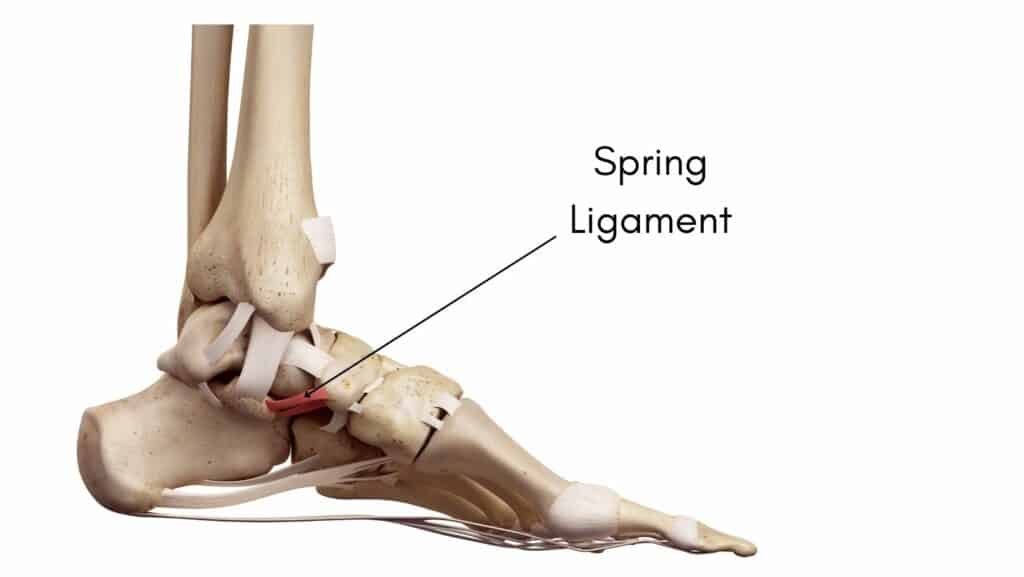
The Spring Ligament (Plantar Calcaneonavicular ligament) is a thick and wide band of cartilaginous connective tissue positioned on the underside of the foot connecting the calcaneus bone to the navicular bone.
The function of the Spring Ligament is to provide stability to the underside of the foot and the foot’s medial arch alongside the Posterior Tibial Tendon. The Spring ligament also resists forefoot abduction. Ligaments attach bone to bone, and alongside the Posterior Tibial Tendon, the Spring Ligament helps to maintain and provide stability to the medial arch of the foot.
In a computational model of the foot, a study found that the Spring ligament contributes to 8% of the total ligament contribution to arch stability to the spring ligament, compared with 79.5% for the plantar fascia.
The symptoms of a Spring Ligament injury include pain, bruising and swelling on the underside of the foot. Pain is worse when weight-bearing as it places the spring ligament under a stretch, while activities such as walking, running or jumping can further exacerbate pain levels.
As the Spring Ligament is instrumental to the stability of the arch of the foot, if it becomes torn, it can lead to a visible reduction in the medial arch height of the foot, causing an Adult flat foot deformity (AFFD).
Alongside an AFFD, it is common to have late-stage Posterior Tibial Tendon dysfunction that may cause pain on the inside of the ankle joint as well as pain on the medial arch of the foot.
There have been some rare cases reported of isolated spring ligament injury, leading to flat foot deformity, with a normal functioning Posterior Tibial Tendon. These patients can normally do a complete heel raise with calcaneal inversion.

Spring Ligament injuries can occur due to various factors, such as repetitive strain from overuse, trauma and medical conditions. These factors can cause irritation and breakdown of the Spring ligament fibres, causing inflammation and pain.
Activities such as running, jumping and dancing can increase your risk of Spring Ligament injury and athletes, dancers and gymnasts have a higher risk of injury.
In some instances, such as a fall from a height, there may be an acute tear or rupture of the Spring ligament. Others may have systemic conditions such as Rheumatoid arthritis which can increase your risk of injury.
Weakness to the Posterior Tibial Tendon can cause an adult-acquired flat foot and place extra stress on the Spring ligament. It can attenuate and stretch the Spring Ligament, resulting in a slow progressive tear.
If you suspect that you have a Spring Ligament injury, we recommend that you have a consultation with a Physical Therapist or a Podiatrist. A physical examination can identify a spring ligament injury using the Neutral Heel lateral push test.
To perform the Neutral Heel Lateral Push test, the clinician positions the patient’s ankle joint in full dorsiflexion and the subtalar joint in neutral. Using the palm of one hand, the clinician stabilises the lateral aspect of the calcaneus. Then, with the other hand, the clinician applies lateral force against the medial aspect of the distal first metatarsal, pushing the forefoot laterally until reaching a firm endpoint.
In this test, one compares the total transverse plane abduction of the forefoot on the rear foot to the contralateral foot. A lack of a firm endpoint may also suggest spring ligament rupture.
It is common for a clinician to refer for imaging to rule out other conditions associated with a Spring ligament injury, such as midfoot arthritis and Posterior Tibial Tendonitis. An MRI is the best scan to identify a Spring Ligament injury.

There are numerous factors to consider when approaching treatment for Spring Ligament injury. Physical Therapy is the most effective form of conservative treatment for a Spring Ligament injury and should factor in the presence of Posterior Tibial Tendon Dysfunction.
Assessing the strength, flexibility and mobility of the foot and ankle helps a therapist create a rehabilitation protocol for a Spring Ligament injury consisting of balance and strengthening exercises.
A gait analysis can identify the necessity for a custom insole that can support the foot’s arch, or advice on the best type of shoe to support your foot type can be helpful.
Home management can include reducing your step count and overall time on your feet while applying ice to the affected area for 15-20 minutes daily for pain relief and taking anti-inflammatories such as Ibuprofen to reduce inflammation in the ligament.
In severe cases, a patient may be advised to spend a period in a walker boot to help offload the foot. After removing the boot, 4-6 weeks of Physical Therapy are carried out to help return the patient to normal functional levels.
Other treatment methods that can be discussed with your therapist is Platelet Rich Plasma (PRP) or surgical reconstruction of the ligament.
A Spring ligament takes 4-6 weeks to heal in mild cases, while in severe cases, it can take 3-6 months for a Spring Ligament to heal.
The spring ligament supports the medial longitudinal arch of the foot. Alongside the Posterior Tibial Tendon, the Spring Ligament plays a vital role in maintaining the structural integrity of the foot.
Yes, you can tear the spring ligament. The most common type of tear is a slow progressive tear that results from an adult-acquired flat foot, but it is possible to tear a Spring Ligament from running or landing from a fall.
A study found 10 patients with acquired flatfoot deformity due to spring ligament injury WITHOUT tibialis posterior tendon tear. Clinically, these cases presented with the following:
– mild to moderate hindfoot valgus
– pain extending from the tip of the medial malleolus to the tarsal navicular
– oedema between the sustentaculum tali and the inferomedial portion of the navicular
– interestingly, all patients we able to achieve a single leg heel raise.
This is not medical advice, and we recommend a consultation with a medical professional such as James McCormack before trying these exercises or treatment recommendations. James offers Online Physiotherapy Appointments weekly.
Related Article: Posterior Tibial Tendonitis