Plica Syndrome Exercises
Read More >
The plica is a folded membrane that sits between the synovial membrane of the tibiofemoral joint and the patella. There are 4 plicae, each a distinct fold: suprapatellar, mediopatellar, infrapatellar and lateral plicae. The membrane when healthy is usually thin, elastic and flexible, with a good blood supply.
At the top of the knee, it is attached to the genu articularis muscle. Inferiorly it blends into the synovial membrane of the tibiofemoral joint. When healthy it can change shape as the knee bends and straightens to prevent it from catching or becoming impinged.
The plicae are the remnant of the 3 separate compartments of the knee that are present as the foetus develops in vitro. The membrane becomes partially absorbed during foetal development but leaves the folds. The plica is noted in surgery in almost everyone but can be more prominent in some people.
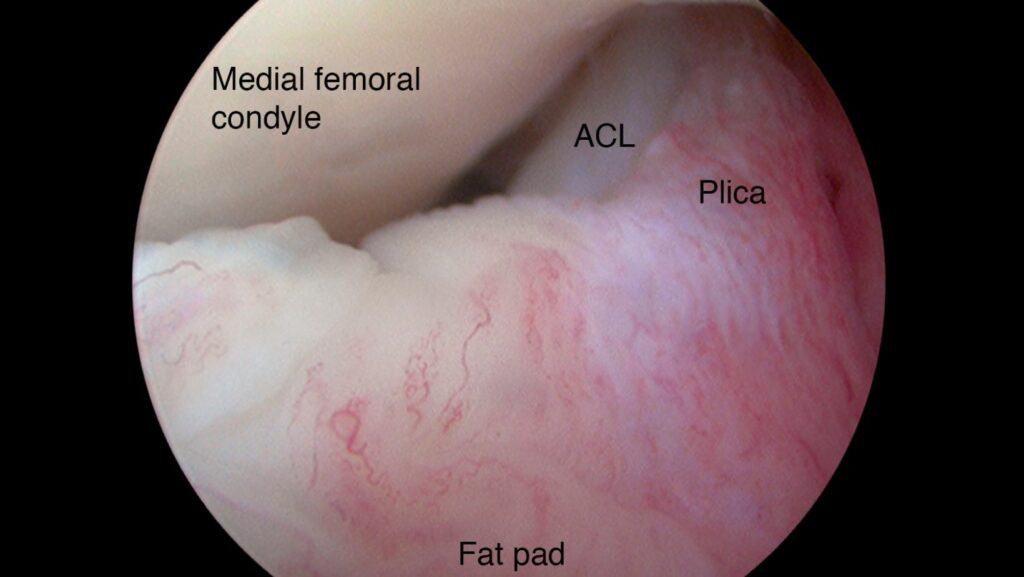
Plica syndrome is a painful condition of the knee, where the synovial membrane has become thickened, fibrotic and less flexible. It therefore is less able to change shape as the knee bends and straightens. It can catch or become impinged, thus becoming inflamed and painful.
This can be triggered by injury, such as a sudden trauma, or overuse, or related to surgery and the resultant scarring of the plica. The medial patella plica is the most commonly affected. This is most vulnerable when the knee is flexed between 70-100º.
The most common symptom of plica syndrome is pain in the knee. The location of pain will be felt deep in the joint. It may not feel clearly in one place, but more generally felt on the inner side of the knee. Pain can be worse at night when the body undergoes repair processes as we sleep.
There is often diffuse swelling of the knee caused by inflammation and joint effusion. Clicking or popping in the knee is frequently felt when the knee is bent or straightened. It can be uncomfortable to sit for long periods of time. Squatting or climbing stairs can aggravate pain. Instability is commonly felt when on a slope or stairs. As these symptoms are similar to many musculoskeletal knee conditions, it is thought to be significantly underdiagnosed.
One of the more unique symptoms is a lump or lesion felt over the affected part of the plica. For example, with a medial patella plica inflammation, can be felt at the front of the knee in the recess between the patella and the medial joint line. Running your finger along this area, you might be able to feel a band or cord-like structure in this area.
If plica syndrome is suspected, a physical examination with an experienced healthcare professional such as a physical therapist or sports doctor is recommended.
They will look at your strength and flexibility. And stress different structures in the knee with clinical tests. These orthopaedics tests will identify sensitive structures and how your knee is functioning.
To confirm a clinical diagnosis, diagnostic imaging such as ultrasound can be used. These images of the plica can show changes to suggest inflammation, thickening or fibrosis. MRI has a sensitivity of 0.77 and a specificity of 0.58.

Part of the clinical assessment will include a diagnostic test specific to the plica. The medial plica syndrome test is performed with the patient lying supine, leg straight and relaxed.
The area medial to the patella is palpated from the lower to the upper part of the cavity. If a cord-like structure is felt that is sensitive, and the patient reports this as their symptom, the test is positive.

Plica syndrome is common after trauma or surgery on the knee. This can be sudden or chronic overload. Such as an increase in volume or intensity of exercise, like running, squatting or going up and down stairs a lot more.
Alternatively, direct acute trauma to the knee can be a cause. Common causes of plica syndrome are a fall onto the knee, or impact on the dashboard in a car accident.
Surgery can cause plica syndrome. An injury to the plica during a surgical procedure and the scarring of the plica after, can cause it to thicken and become fibrotic. After knee replacement, ACL reconstructive surgery and knee arthroscopy, plica syndrome is a reported risk.
In terms of age, most cases occur between the ages of 10-30 years. There is an even distribution between men and women. Genetics may play a role in the development of plica syndrome. Genetics can influence the shape and depth of the folds, and the flexibility of the membrane. There is limited evidence to confidently conclude this, however.
The recovery time from plica syndrome is typically 4-6 weeks. If conservative management is not effective, steroid injections and or surgery may be offered. Healing time after surgery is typically 4-6 weeks.
Physical therapy and a specific programme of rehabilitation exercises is the best treatment. And it is effective in most cases.
You can read more about specific exercises and stretches to do as well as exercises to avoid in our related article: Plica Syndrome Exercises.
The use of tape or strapping is widely used by therapists and individuals for this condition. It can be a helpful way to reduce pain.
This temporary pain reduction can help individuals perform their rehabilitation exercises and daily activities.
Medication can be taken if pain levels are high or if symptoms are not settling. Typically, non-steroidal anti-inflammatories are prescribed for pain relief and to reduce inflammation.
If conservative treatment is not effective, cortisone injections may be recommended. Cortisone is a powerful steroid for reducing inflammation. It can help the inflamed plica to settle down.
Steroid injections should be done cautiously as steroids can do harm to the body. In some tissues, it can cause a breakdown and weakening of their structure.

Plica syndrome surgery recovery is relatively quick, typically 4-6 weeks. It is a simple procedure where the plica is either completely or partially removed. The knee can function completely normally without the plica. Therefore, there is no adverse effect from surgery, aside from the trauma of getting into the knee.
This article is written by James McCormack, a Lower Limb Specialist who is an expert in treating Plica Syndrome.
This is not medical advice. We recommend a consultation with a medical professional such as James McCormack if you are experiencing any of the symptoms discussed in this article. James offers Online Physiotherapy Appointments weekly and face-to-face appointments in his London clinic.