PCL Tear Symptoms, Causes and Diagnosis
Read More >
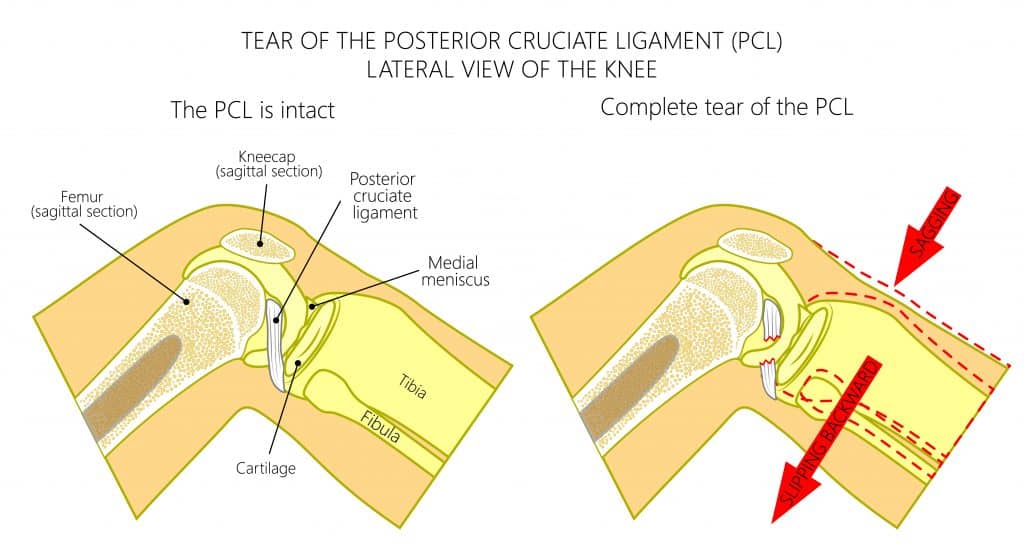
The PCL is the posterior cruciate ligament of the knee. It is the strongest ligament in the knee and one of the 4 main stabilising ligaments for the knee joint.
The PCL is attached to the femur and the tibia bones, it is angled down and back from the femur to the tibia at about 123º. This direction between its origin and insertion means that the PCL functions to stop the tibia from moving posteriorly relative to the femur.
Most people are still able to walk with a torn PCL, provided that the severity of the tear is low. Higher-grade tears are related to more ligament damage, with a grade 3 classification for a full rupture. The greater the damage, the greater the chance that there will be instability of the joint, and worse pain.
Similarly to walking, it depends on the severity of the injury. But as running is a high impact exercise, any pain or instability felt with walking will be worse with running. When recovering from a PCL injury and returning to running, may people will be advised to use taping or strapping or to wear a structured knee brace.
In most cases, surgery is not needed to treat a PCL. Surgery is only recommended for grade 3 tears which are complete or near-complete ruptures which also have significant instability of the joint. In these cases, surgery might be offered if there is no improvement in the symptoms of instability after a course of physiotherapy and the use of a brace for 6 weeks.

After surgery, there is a long road of rehabilitation, which is usually 10-12 months to return to sport, but can be more. The initial few days after surgery will be the most painful, and getting swelling and pain under control is the aim for this period. Take the recommended medication, and elevate and ice your knee regularly during the day.
Seeing a physical therapist to guide your rehabilitation from early on is key. Starting mobility exercises in the first few days will help you to recover full range of movement quickly. During this phase, you will also be encouraged to start activation of the muscles around your knee, such as your quadriceps.
Progressively more difficult strengthening exercises, balance, movement control and impact exercises will follow, over the following weeks and months, to return you to the activities that you enjoy.
The body takes time to recover, and that cannot be sped up beyond a certain point. To ensure the most efficient healing to occur, you need to provide the best environment for your body to heal, and the best stimulation for the tissues to repair and strengthen.
Sleep more: Sleep is undoubtably one of the most important factors that can affect tissue healing time. There have been many studies on this subject, the results of one showed that just one night of sleep deprivation increase cortisol levels by 21% and reduced testosterone by 24% skeletal muscle protein synthesis by 18% (Lamon et al, 2021).
Eat well: A healthy, varied diet, that is macronutrient balanced and micronutrient rich, will ensure your body has the fuel and building blocks to repair.
Don’t drink alcohol or smoke: Alcohol and nicotine are substances that have been well researched substances that slow down healing.

This is not medical advice. We recommend a consultation with a medical professional such as James McCormack. He offers Online Physiotherapy Appointments for £45.